Featured
- Get link
- X
- Other Apps
Empire Blue Cross Blue Shield Prior Authorization
Please check your schedule of benefits. Please be advised that these.
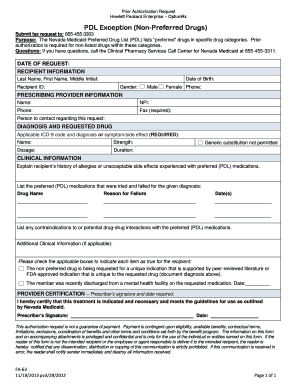 2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
Wants to remind providers.

Empire blue cross blue shield prior authorization. Services provided by Empire HealthChoice HMO Inc. If you do not get approval from Blue Cross and Blue Shield of Vermont before administration. Empire will waive member cost shares for COVID-19 lab tests performed by participating and non-participating providers.
Fill out securely sign print or email your blue cross blue shield of alabama prior authorization form instantly with signNow. Start a free trial now to save yourself time and money. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Install the signNow application on your iOS device. For information on precertification requirements for those members of National. Empire BlueCross BlueShield.
Available for PC iOS and Android. If benefit prior authorization is required services performed without benefit prior authorization or that do not meet medical necessity criteria may be denied for payment and the rendering provider may not seek reimbursement from the member. Upload the PDF you need to e-sign.
The most secure digital platform to get legally binding electronically signed documents in just a few seconds. NYE-NU-0321-21 May 2021 Correction to a prior authorization update In a recent notification we shared that effective May 1 2021 the following codes would be included in our prior authorization review process. The following guidelines apply to Anthem Blue Cross and Blue Shield Anthem products issued and delivered by Anthem in New Hampshire.
This is called prior approval precertification or preauthorization. Empire BlueCross BlueShield HealthPlus Empire is available via phone or the Interactive Care Reviewer ICR 24 hours a day 7 days a week to accept prior authorization PA requests. To sign a hipaa individual authorization empire blue cross blue shield right from your iPhone or iPad just follow these brief guidelines.
The Blue Cross and Blue Shieldnames and symbols and registered marks of the Blue Crossand Blue Shield Association Revised 07262019 Prior authorizationPreservice clinical review is required through AIM for the following non-emergent outpatient services. In some situations you need to get your care treatment or prescription drugs approved before we cover them. No prior authorization is not required for diagnostic services related to COVID-19 testing.
The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Please complete this form and fax or mail to. When prior authorization is required you can contact us to make this request.
That they are required to request a prior authorization for Medicare Advantage members for services that require prior authorization. Providers should continue to verify eligibility and benefits for all members prior to rendering services. You can access the ICR from the Availity home page.
The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. Anthem has also made available a series of. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required.
Outpatient Prior Authorization CPT Code List 072 Prior Authorization Quick. This approval process is called prior authorization. Andor Empire HealthChoice Assurance Inc licensees of the Blue Cross and Blue Shield Association an association of independent Blue Cross and Blue Shield Plans.
Prior review prior plan approval prior authorization prospective review or certification is the process Blue Cross NC uses to review the provision of certain behavioral health medical services and medications against health care management guidelines prior to the services being provided. Does Empire require use of a contracted provider for the COVID-19 lab test in order for waiver of the members cost share to apply. Create an account using your email or sign in via Google or Facebook.
Use the Prior Authorization tool within Availity or Call Provider Services at 1-800-450-8753 TTY 711 After hours verify member eligibility by calling the 247 NurseLine at 1-800-300-8181. The ICR allows detailed text photo images and attachments to be submitted along with your request. Empire BlueCross Blue Shield Prior Authorization Required for Members.
Some drugs and certain amounts of some drugs require an approval before they are eligible to be covered by your benefits. List of services drugs and supplies that require approval from Blue Cross and Blue Shield of Vermont prior to administration andor admission. Anthem Blue Cross and Blue Shield in New Hampshire.
Drug listFormulary inclusion does not infer a drug is a covered benefit. PRIOR AUTHORIZATION REQUEST FORM REQUESTED AGENT. For some services listed in our medical policies we require prior authorization.
Failure to obtain a prior authorization will result in an administrative denial. The 2015 prior authorization requirements were. Empire BlueCross BlueShield HealthPlus is the trade name of HealthPlus HP LLC an independent licensee of the Blue Cross and Blue Shield Association.
 Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Https Www Anthem Com Provider Noapplication F4 S6 T0 Pw E213404 Pdf Refer Ahpprovider State Ct
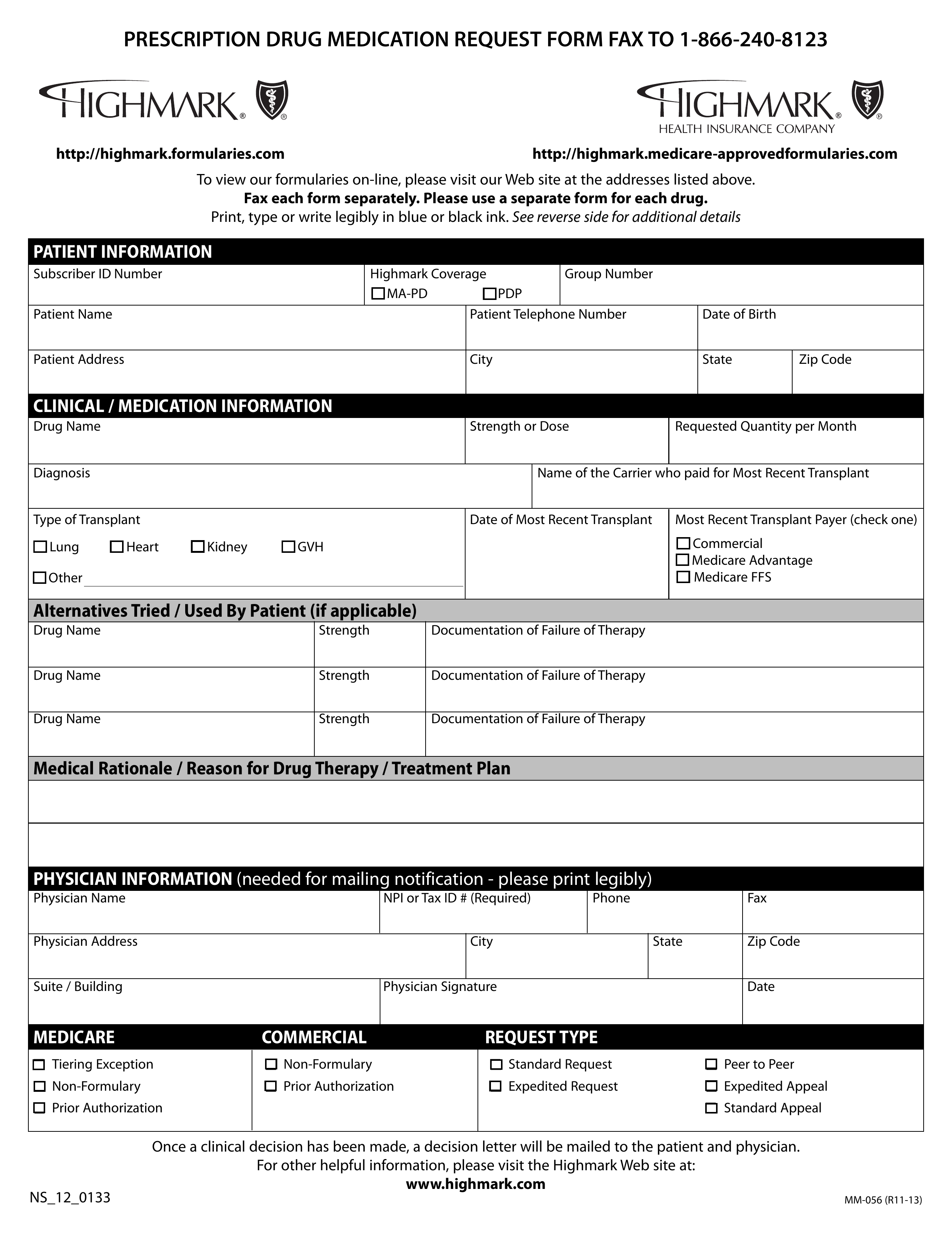 Free Highmark Prior Rx Authorization Form Pdf Eforms
Free Highmark Prior Rx Authorization Form Pdf Eforms
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E228625 Pdf Na Pharminfo
 Anthem Blue Cross Prior Authorization Form Fax Number Inspirational 20 Unique Express Scripts Prior Authorization Form Medicare Part D Models Form Ideas
Anthem Blue Cross Prior Authorization Form Fax Number Inspirational 20 Unique Express Scripts Prior Authorization Form Medicare Part D Models Form Ideas
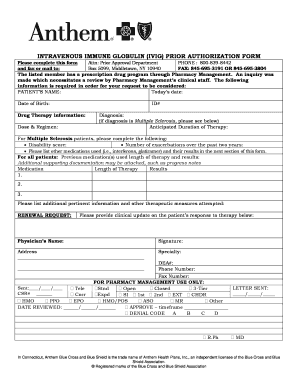 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Https Www Empireblue Com Provider Noapplication F1 S0 T0 Pw E244518 Pdf Refer Ehpprovider
Https Www Anthem Com Provider Noapplication F1 S0 T0 Pw Ad080665 Pdf Refer Ahpprovider
 Anthem Blue Cross Prior Authorization Form Fax Number Inspirational Blue Cross Blue Shield Federal Plan Brochure Inspirational 2018 Vw Models Form Ideas
Anthem Blue Cross Prior Authorization Form Fax Number Inspirational Blue Cross Blue Shield Federal Plan Brochure Inspirational 2018 Vw Models Form Ideas
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
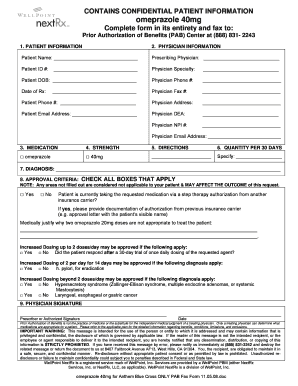
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
 Anthem Blue Cross Medi Cal Prior Authorization Form Lovely Optum Rx Prior Authorization Form Templates Optumrx Best Hello Models Form Ideas
Anthem Blue Cross Medi Cal Prior Authorization Form Lovely Optum Rx Prior Authorization Form Templates Optumrx Best Hello Models Form Ideas
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment