Featured
- Get link
- X
- Other Apps
Cvs Specialty Pharmacy Prior Authorization
Prior authorization and drug eligibility review. CVS Specialty Pharmacy will assist you in filling your patients specialty drug.
Https Hmsa Com Portal Provider Cvs Xoliar Prior Auth 112011 Pdf
Specialty Pharmacy Services Information and Forms.
Cvs specialty pharmacy prior authorization. Access to a broad inventory of injectable infused and oral specialty medications. Required clinical information - Please provide all relevant clinical information to support a prior authorization or step therapy exception request review. Delivery to home physicians office or infusion site.
Specialty pharmacy provider CVScaremark. In doing so CVSCaremark will be able to decide whether or not the requested prescription is included in the patients insurance plan. In 2020 alone the US.
CVS was a great place to work for good management. Eastern Monday Friday. A specialty pharmacy is a provider of complex medications for complex health conditions.
We work with providers to streamline prior authorization for prescriptions and with insurance companies to verify benefits coverage. Apply on company website Save. Pharmacy Technician prior authorization rep Former Employee - Raleigh NC - April 27 2021.
Obtaining Specialty Drug Authorizations for Members with a Non-Medicare HMO Plan BlueCare HMO myBlue and SimplyBlue CVS Caremark will review and provide authorization for specialty drug requests on our behalf. Injected or infused. Food and Drug Administration approved 34 new specialty treatments 64 percent of all approvals and 81 supplemental indications spanning 33 conditions.
Prior Authorization can ensure proper patient selection dosage drug administration and duration of selected drugs. CVS Caremark Prior Authorization PA tools are developed to ensure safe effective and appropriate use of selected drugs. Contact the atspecialty pharmacy provider or CVScaremark 866 814-5506 for questions.
Contact CVS Specialty Pharmacy at 1-800-237-2767 from 730 am. A lot of changes to get use to. Prior Authorization Pharmacy Technician CVS Health Phoenix AZ 3 days ago Be among the first 25 applicants.
CVS Caremark is dedicated to helping physicians manage and help their patients who are suffering from complex disorders and require specialized therapies and personalized care. How do I obtain a prior authorization for Actemra Download a prior authorization fax form send to 866 249-6155. Empire FEP will begin accepting prior authorization requests for these specialty drugs on December 14 2020 for dates of service on and after January 1 2021.
Medications handled by a specialty pharmacy may be. Specialty Expedite uses digital tools to help get patients started on new medications quickly. This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered.
June 2019 As the fastest growing area of pharmacy spend effectively managing specialty treatments is the biggest pain point for payors and their members and many are looking for ways to aggressively control costs. In addition to that a specialty pharmacy also helps people manage their health. CVS Caremark is launching a pilot of a real-time integrated electronic prior authorization ePA capability that will be available to CVS Caremark Pharmacy Benefit Management PBM clients to help improve the patient experience and speed access to prescription medications.
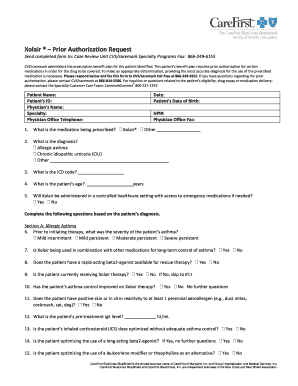
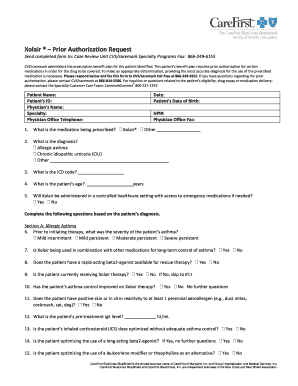
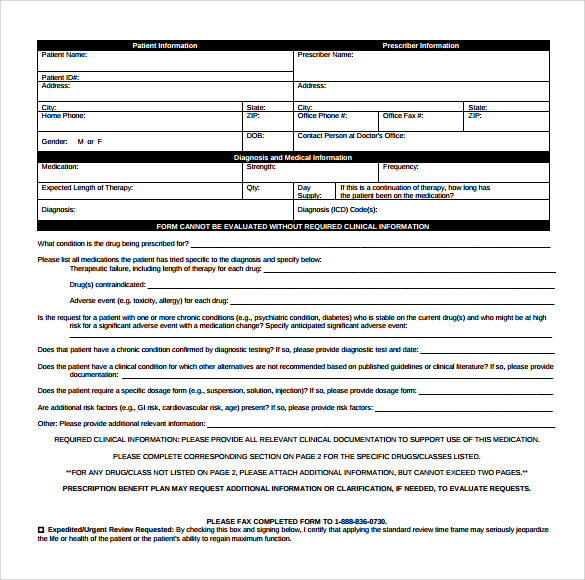
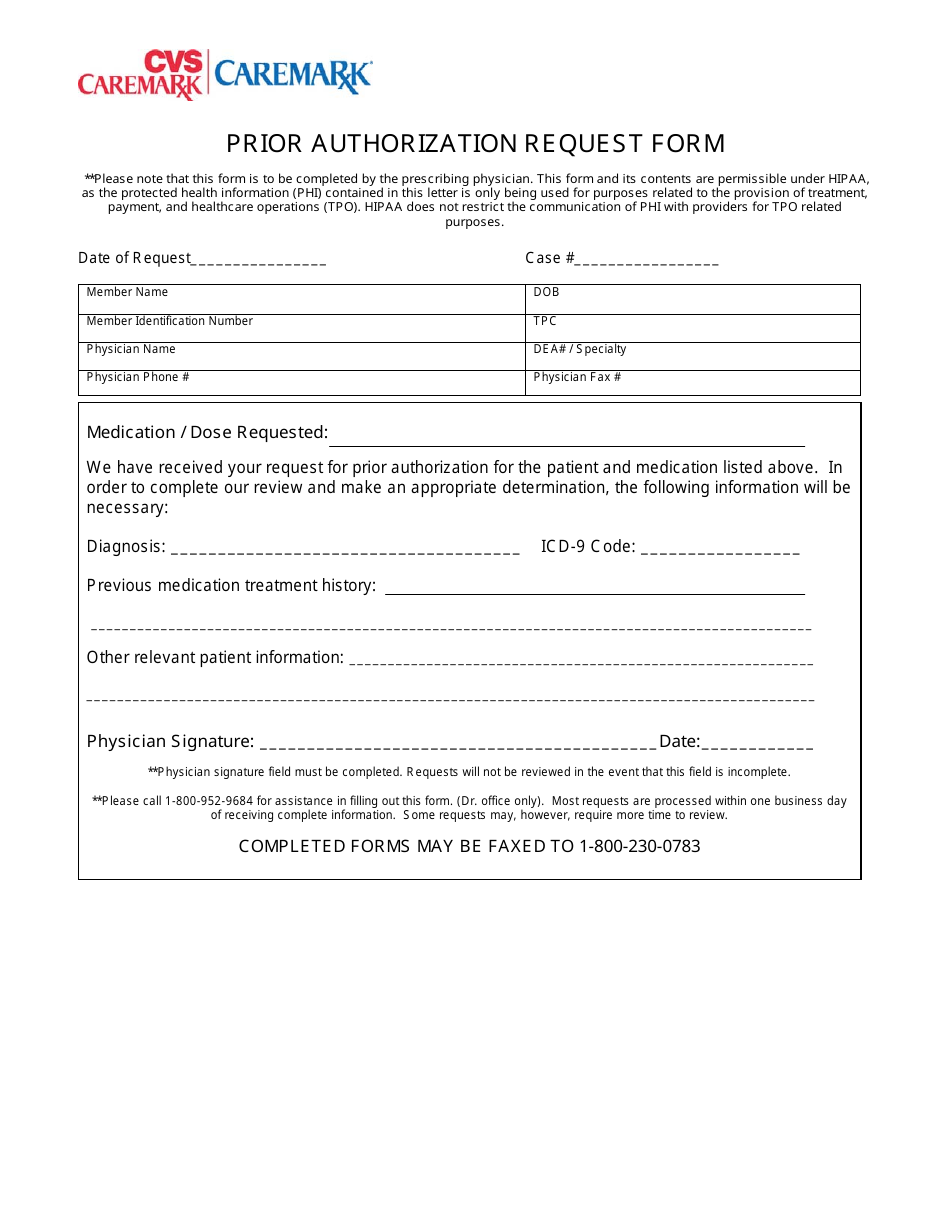
To make an appropriate determination providing the most accurate diagnosis for the use of the. You can check our health plan website. HMSA - Prior Authorization Request CVS Caremark administers the prescription benefit plan for the patient identified.
CVS speciality taught me a lot on the pharmacy side about specialty meds. The CVSCaremark prior authorization form is to be used by a medical office when requesting coverage for a CVSCaremark plan members prescription. Prior Authorization PA still applies to specific specialty drugs.
Apply to Prior Authorization Specialist Pharmacy Technician Authorization Specialist and more. Request prior authorization review by calling the Blue Cross and Blue Shield Federal Employee Program Service Benefit Plan at 800 860-2156. Together we can help more people lead longer and healthier lives.
Apply to Prior Authorization Specialist Pharmacy Technician Authorization Representative and more. See who CVS Health has hired for this role. Our CarePlus Specialty Pharmacy specializes in Oncology MS Hepatitis HIV Rheumatology Dermatology and Transplant and Gastrointestinal diseases.
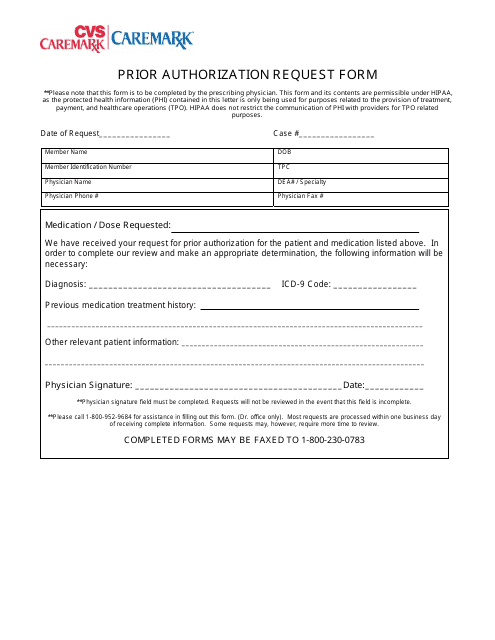
CVS Health has an exciting new opportunity for a Prior Authorization Specialist - Pharmacy Technician in New York NY. Please provide symptoms lab results with dates andor justification for initial or ongoing therapy or increased dose and if patient has any. A physician will need to fill in the form with the patients medical information and submit it to CVSCaremark for assessment.
If you would like to view forms for a specific drug visit the CVSCaremark.
 Fillable Online Global Prior Authorization Form Cvs Caremark Fax Email Print Pdffiller
Fillable Online Global Prior Authorization Form Cvs Caremark Fax Email Print Pdffiller
Https Member Carefirst Com Carefirst Resources Provider Pdf Drug Ofev Sgm Pdf
 Cvs Caremark Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Cvs Caremark Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
 Cvs Caremark Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Cvs Caremark Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
 Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
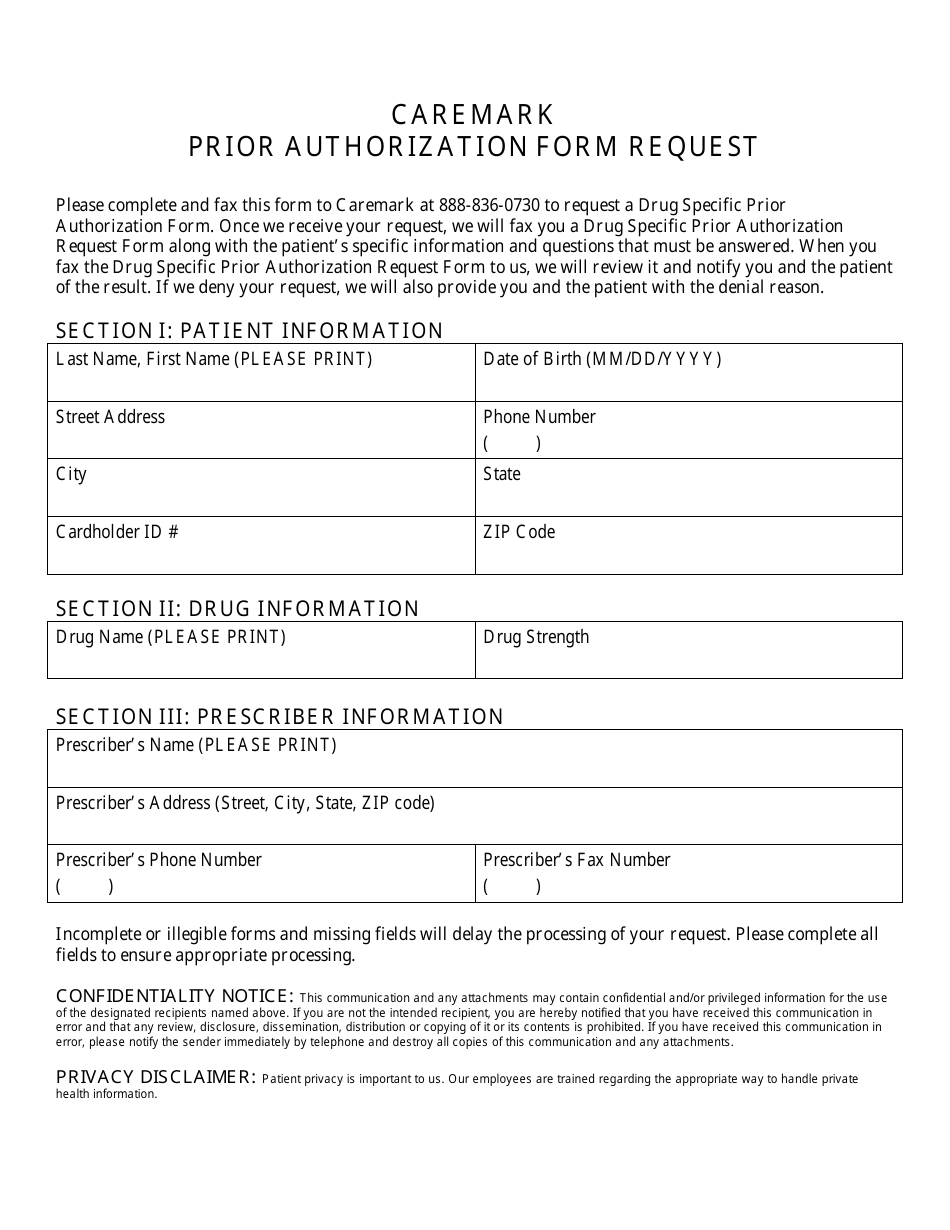 Prior Authorization Form Request Cvs Caremark Download Printable Pdf Templateroller
Prior Authorization Form Request Cvs Caremark Download Printable Pdf Templateroller
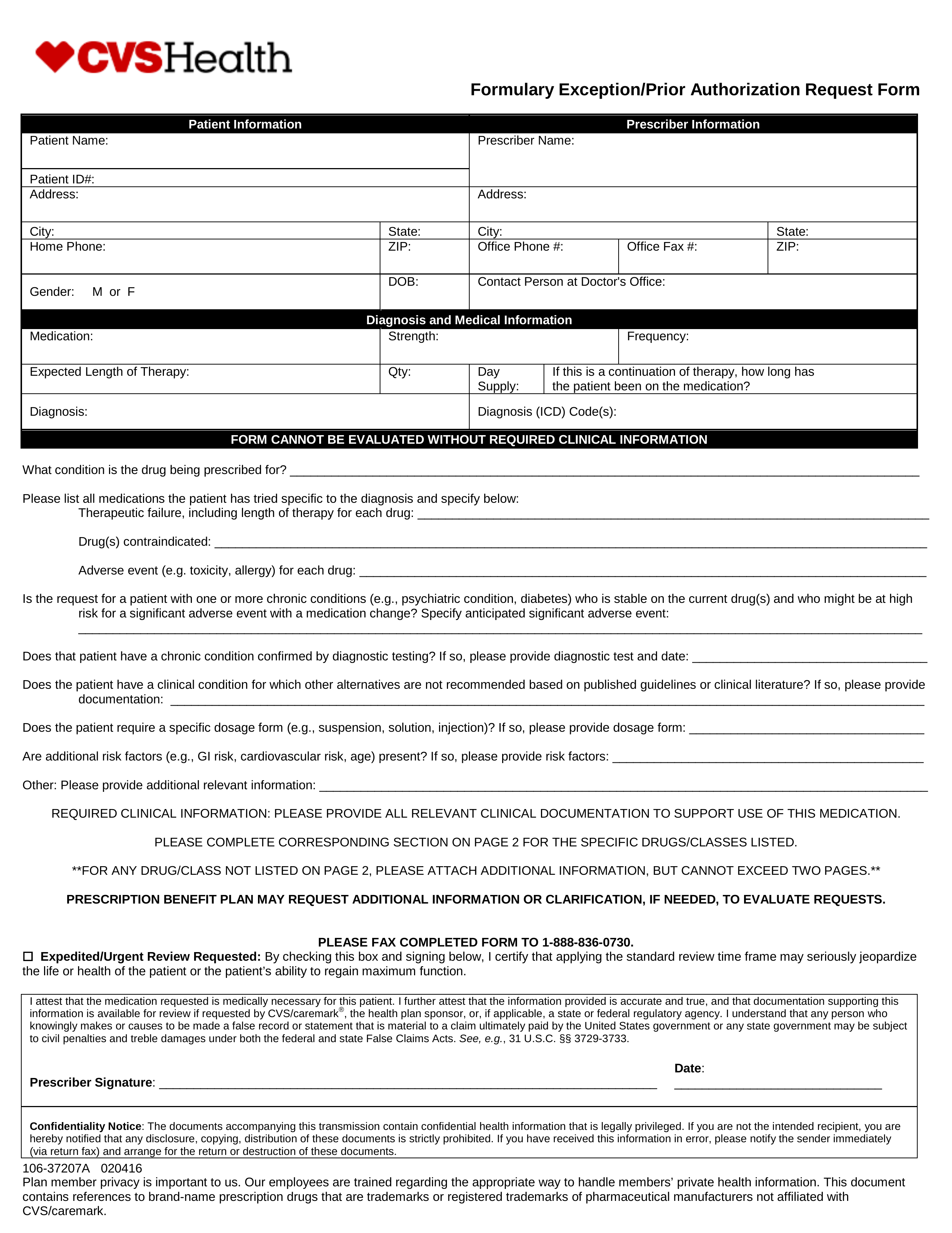 Free Cvs Caremark Prior Rx Authorization Form Pdf Eforms
Free Cvs Caremark Prior Rx Authorization Form Pdf Eforms
 Cvs Caremark Prior Authorization Form 600x800 Free Job Application Form
Cvs Caremark Prior Authorization Form 600x800 Free Job Application Form
 Cvs Caremark Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Cvs Caremark Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
 Free 8 Sample Caremark Prior Authorization Forms In Pdf
Free 8 Sample Caremark Prior Authorization Forms In Pdf
Http Www Ultrabenefits Com Sitecore Content Fallon Total Care Providers Pharmacy Media Ftc Pharmacyforms Ftc Caremarkpriorauthform Ashx
 Cvs Caremark Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Cvs Caremark Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
 Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
 Cvs Specialty What Is A Prior Authorization
Cvs Specialty What Is A Prior Authorization
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment