Featured
Does My Blue Cross Blue Shield Cover Therapy
To verify your addiction treatment coverage click here or use the form below. For children under age 12 HMO Blue and Blue Choice covers preventive dental care when provided by a Blue Cross Blue Shield of Massachusetts participating dentist.
 Does Blue Cross Blue Shield Cover Therapy Drug Rehab
Does Blue Cross Blue Shield Cover Therapy Drug Rehab
The answer is yes but not to an unlimited extent.
Does my blue cross blue shield cover therapy. Yes the vast majority of Blue Cross Blue Shield plans cover therapy. The therapist you wish to see needs to accept Blue Cross Blue Shield insurance. Many also have a sequence of biologic drugs that must be used.
Blue Care Network members under age 65. First Care Inc and The Dental Network Inc. Hospital Emergency Room Visits.
The vast majority of Blue Cross Blue Shield insurance plans cover therapy. Does Blue Cross Blue Shield Cover Therapy. Laboratory and X-ray Services.
Blue Shield is one of the therapy providers whose plan covers in-office therapy and online therapy treatments. All medically necessary lab services. In the case of an eating disorder your health care provider may recommend a total rehabilitation program and the insurance company will.
Many plans also cover medications to treat mental health. Hospital Inpatient Services and Ambulatory Services. Some Blue Cross Blue Shield employers offer mental health benefits.
Yes these services must be ordered by your PCP. Does insurance like Blue Shield cover therapy. Blue Cross and Blue Shield of Texas a Division of Health Care Service Corporation a Mutual Legal Reserve Company Southwest Texas HMO Inc dba HMO BlueÒ Texas Independent Licensees of the Blue Cross and Blue Shield Asso ciation COVERAGE.
Heres how to get those services and find out. If however your plan started before 2014 when the Affordable Care Act was enacted your plan may not cover therapy. Blue Cross and Blue Plus health plans typically cover behavioral and mental health services.
How much is therapy out of pocket. For example MTX Soriatane Phototherapy is usually used before a patient is biologic eligible. All of their plans follow the guidelines of the Affordable Care Act ACA and provide individuals with the same.
Theyre part of your behavioral health coverage. Electroconvulsive therapy ECT may be eligible for coverage for patients who. There may be reasons why the therapist of your preference does not accept BCBS insurance so if this is the case speak to your therapist of choice about alternatives.
This includes one initial exam per child followed by one periodic exam every six months one cleaning every six months one fluoride treatment every six months and bitewing X-rays every six months. BLUE CROSS BLUE SHIELD and the Cross and Shield Symbols are registered service marks of the Blue Cross and Blue Shield Association an association of independent Blue Cross and Blue Shield Plans. All Fields Required Find Insurance Carrier 1.
I step-edit is a specific sequence of treatments that must be completed to qualify for drug coverage. Blue Cross Blue Shield requires adherence and will only cover a medically necessary PAP device beyond the first three months of therapy when PAP use is greater than or equal to 4 hours per night on 70 of nights during a consecutive 30 day period during the first three months of therapy. Most BCBS plans will have a step-edit in place and require strict adherence.
Blue Cross Blue Shield is a major provider whose insurance covers mental health. Most plans offer 12 therapy sessions per calendar year unless additional treatment is recommended by a health care provider. Health insurances offered through the Marketplace or through small employers are required by the Affordable Care Act to cover mental health services and while not required by federal law the vast majority of large employers also cover mental health services.
Blue Cross and Blue Shield of Florida Blue Cross Blue Shield or BCBS is an insurance provider that may offer coverage for substance abuse and mental health treatment. Are independent licensees of the Blue Cross and Blue Shield Association. The Recovery Villages national network of centers offers comprehensive treatment and therapy to help you establish a life built on principles of self-worth and sobriety.
The amount of Blue Cross Blue Shield therapy coverage you receive is based on many factors including the type of coverage you have the state in which you live and your particular insurance plan. Blue Cross Blue Shield offers bronze silver and gold insurance plans for individuals and families businesses and federally employed individuals. Go to the nearest hospital in an emergency.
Fortunately almost all BCBS insurance programs include coverage for mental health and substance-use disorders. Blue Cross Blue Shield requires adherence and will only cover a medically necessary PAP device beyond the first three months of therapy when PAP use is greater than or equal to 4 hours per night on 70 of nights during a consecutive 30 day period during the first three months of. Blue Cross Blue Shield requires adherence and will only cover a medically necessary PAP device beyond the first three months of therapy when PAP use is greater than or equal to 4 hours per night on 70 of nights during a consecutive 30 day period during the first three months of therapy.
The Blue Cross and Blue Shield Association covers every major physical and mental health issue. Blue Care Network plans cover or help pay for mental health and substance use disorder services. The services covered for inpatient or outpatient care the copays or coinsurance amounts and the network of providers may be different for each plan.
 Does Insurance Cover Therapy When How To Check And More Tips
Does Insurance Cover Therapy When How To Check And More Tips
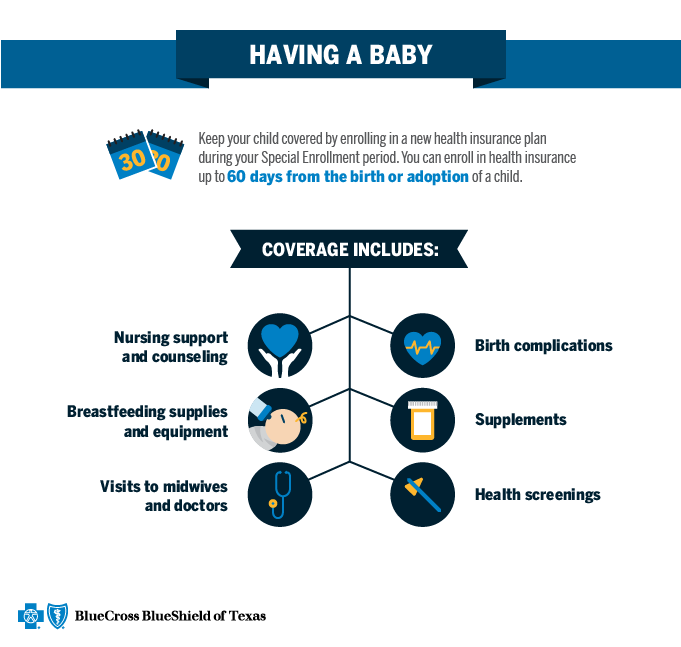 Qualifying Event Baby Blue Cross And Blue Shield Of Texas
Qualifying Event Baby Blue Cross And Blue Shield Of Texas
 Blue Cross Blue Shield For Therapy Zencare Guide Zencare
Blue Cross Blue Shield For Therapy Zencare Guide Zencare
 Summary Of Health Plan Payments Myblue
Summary Of Health Plan Payments Myblue
 Health Plan Overview Blue Cross And Blue Shield S Federal Employee Program
Health Plan Overview Blue Cross And Blue Shield S Federal Employee Program
 Blue Cross Blue Shield Cpap Therapy Policies Health Sqyre
Blue Cross Blue Shield Cpap Therapy Policies Health Sqyre
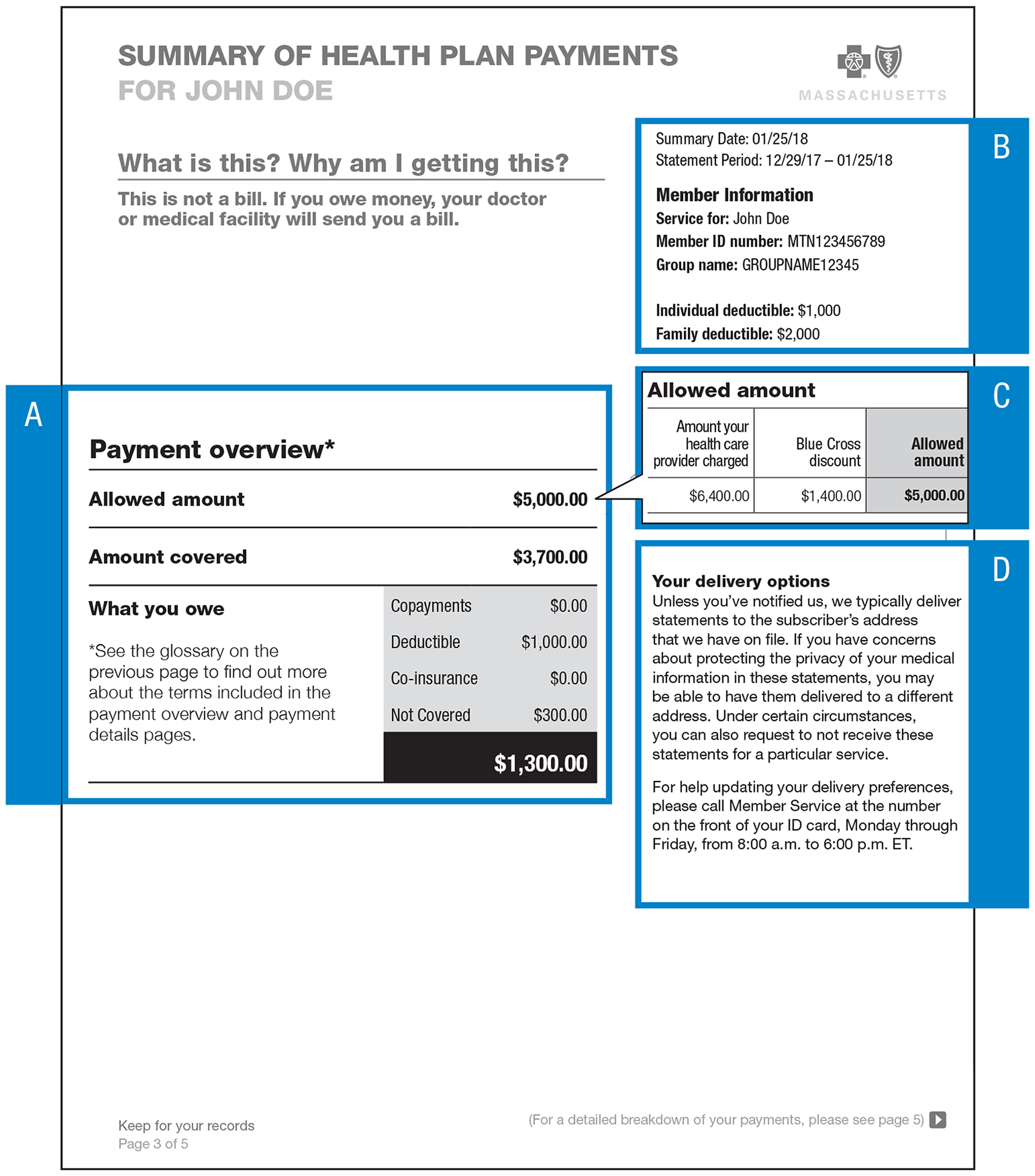 Summary Of Health Plan Payments Myblue
Summary Of Health Plan Payments Myblue
 Ppo Blue Cross And Blue Shield Of Illinois
Ppo Blue Cross And Blue Shield Of Illinois
Https Www Aota Org Media Corporate Files Advocacy Health Care Reform Exchanges Analysis Of Plans Ga Bcbs Pdf
 Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
Https Www Aota Org Media Corporate Files Advocacy Health Care Reform Exchanges Analysis Of Plans Me Anthembcbs Pdf
 Blue Cross Blue Shield Florida Cpap Coverage Health Sqyre
Blue Cross Blue Shield Florida Cpap Coverage Health Sqyre
 Blue Cross Blue Shield For Therapy Zencare Guide Zencare
Blue Cross Blue Shield For Therapy Zencare Guide Zencare
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment