Featured
- Get link
- X
- Other Apps
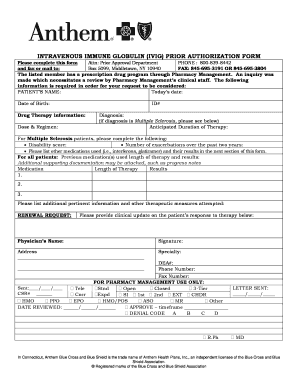
Anthem Prescription Prior Authorization Form
Browse commonly requested forms to find and download the one you need for various topics including pharmacy enrollment claims and more. Prior Authorization Requirements.
 Fillable Online Anthem Prior Auth Request For Form Fax Email Print Pdffiller
Fillable Online Anthem Prior Auth Request For Form Fax Email Print Pdffiller
Select the template in the catalogue.
Anthem prescription prior authorization form. Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location. Looking for a form but dont see it here. Our state-specific online blanks and clear recommendations eradicate human-prone errors.
Follow our easy steps to have your Anthem Prior Authorization Request well prepared rapidly. Get And Sign Anthem Prescription Drug Prior Authorization Request Form For Missouri 2011-2021 Inadequate response to treatment with at least ONE first-line pharmacologic therapy including ONE oral bisphosphonate of adequate treatment duration OR the patient is intolerant or has a contraindication to the use of at least TWO first line pharmacologic agents. Please provide symptoms lab results with dates andor justification for initial or ongoing therapy or.
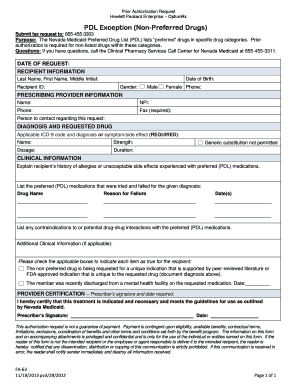
Please fill out the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form and fax. Required clinical information - Please provide all relevant clinical information to support a prior authorization or step therapy exception request review. Provider tools resources.
You may also ask us for a coverage determination by phone at Anthem Blue. The drug specific criteria and forms found within the Searchable lists on the Drug List Search tab are for informational purposes only to assist you in completing the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form if they are helpful to you. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan.
Log in to Availity. 1-800-338-6180 PLEASE COPY THIS FORM FOR FUTURE REQUESTS for Anthem Pharmacy Programs PRIOR AUTHORIZATION NON-FORMULARY EXCEPTIONS REQUEST FORM. Prior Authorization is required and is limited to medically use of medical gases or Prescription Drugs in the form of aerosols and equipment such as.
466 Zeilen The Food and Drug Administration FDA is warning that rare but serious injuries. Anthem Prior Prescription Authorization Form Step 2 Specify the drug name in the top-most field. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Provider Maintenance Form. A library of the forms most frequently used by health care professionals. Anthem has also made available a series of forms.
Anthem prescription prior authorization form. Anthem Utilization Management Services Inc. On the prior authorization form the person making the request must provide a medical rationale as to why the chosen.
Learn about Availity. Anthem Blue Cross and Blue Shield Anthem State Health Benefit. Attention prescribing providers with members enrolled in an Anthem Colorado health plan.
Connecticut - 8444743350 Georgia - 8445129002. We are currently in the process of enhancing this forms library. Step 1 Download in Adobe PDF.
Prior Authorization Lookup Tool. San Antonio TX 78265-8686. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
The Colorado Prescription Drug Prior Authorization Request form may be used to submit prior authorization PA requests for members enrolled in a Colorado health plan regardless of residenceThe preferred method to submit PA requests is through our electronic PA ePA. Provider Forms Guides. Anthem Prescription Prior Authorization Center 8990 Duke Blvd MP2-826 Mason OH 45040 Fax.
Now creating a Anthem Prior Authorization Request requires at most 5 minutes. Anthem Blue Cross Cal MediConnect. The patients personal insurance information their current condition and the previous drugstherapies attempted to remedy their condition must be supplied.
Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptionsA non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State. 2019 SHBP Anthem HRA Summary Plan Description. Medicare Prior Authorization Review.
Please contact us for assistance. The AETNA prescription prior authorization form is a document that is used to justify the prescribing of a particular medication not already on the AETNA formulary. REQUEST FOR MEDICARE PRESCRIPTION DRUG COVERAGE DETERMINATION This form may be sent to us by mail or fax.
During this time you can still find all forms and guides on our legacy site. PRESCRIPTION DRUG PRIOR AUTHORIZATION REQUEST FORM Contains Confidential Patient Information Complete form and fax back accordingly. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost.
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
 Anthem Blue Cross Prior Authorization Form Fax Number Inspirational 20 Unique Express Scripts Prior Authorization Form Medicare Part D Models Form Ideas
Anthem Blue Cross Prior Authorization Form Fax Number Inspirational 20 Unique Express Scripts Prior Authorization Form Medicare Part D Models Form Ideas
 Fillable Online Anthem Prior Authorization Form For Procedures Fax Email Print Pdffiller
Fillable Online Anthem Prior Authorization Form For Procedures Fax Email Print Pdffiller
 Beautiful Anthem Blue Cross Prior Authorization Form Fax Number Models Form Ideas
Beautiful Anthem Blue Cross Prior Authorization Form Fax Number Models Form Ideas
 Anthem Blue Cross Medi Cal Prior Authorization Form Lovely Optum Rx Prior Authorization Form Templates Optumrx Best Hello Models Form Ideas
Anthem Blue Cross Medi Cal Prior Authorization Form Lovely Optum Rx Prior Authorization Form Templates Optumrx Best Hello Models Form Ideas
Https Mss Anthem Com California Mmp Caca Mmp 2020coveragedeterminationform Eng Pdf
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Https Www Anthem Com Ca Provider F3 S1 T4 Pw E224354 Pdf Refer Agent
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E228625 Pdf Na Pharminfo
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
Https Www Anthem Com Provider Noapplication F1 S0 T0 Pw Ad080665 Pdf Refer Ahpprovider
 2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment