Featured
Out Of Network Medicare Advantage
This information is not a complete description of benefits. There are rare instances when providers will encounter a situation where a MA plan enrollee receives or seeks services from a provider that is not part of the MA plans network.
 Medicare Advantage Programs Types Of Medicare Advantage Plans
Medicare Advantage Programs Types Of Medicare Advantage Plans
Out of network coverage for CareFirst Medicare Advantage Medicare Plan.
Out of network medicare advantage. As a precondition for the Provider to. As a member of our plan you can choose to receive care from out-of-network providers. Cigna will reimburse out of network providers that provide Covered Services to its Medicare Advantage plan members in accord with CMS regulations and the members Benefit Plan design.
That is neither the HMO plan nor TM will pay for services when an MA member goes out-of-network. Medicare Advantage Plan Part C offered by a private insurance company. You can also choose an out-of-network doctor other health care provider or hospital that accepts the plans terms but it may cost more.
Enrollment in Health Net Medicare Advantage for Oregon and Washington depends on contract renewal. The payment rates described in this document do not apply to a plans network providers. Our plan will cover services from either in-network or out-of-network providers as long as the services are covered benefits and medically necessary.
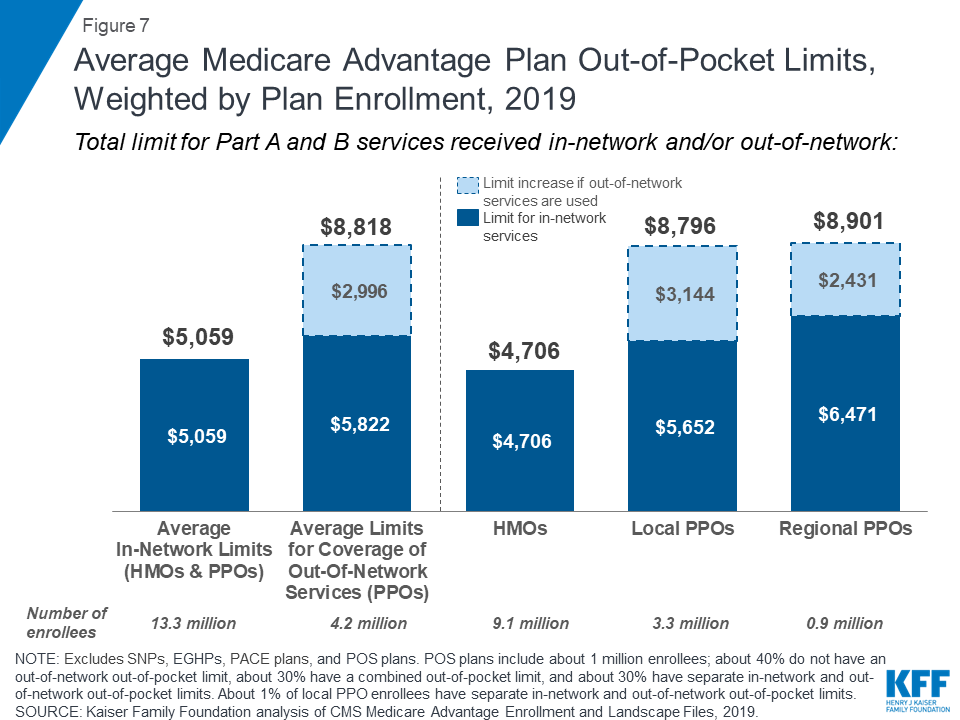
This limit cannot be higher than 7500 for in-network services or 11300 for combined in-and out-of-network services. You pay more if you use doctors hospitals and providers outside of the network. Health Maintenance Organization HMO plans are restrictive about your seeing Medicare doctors in network.
Other than for Medicare beneficiary cost-sharing physicians and other health care providers may not bill Medicare Advantage enrollees for any additional amounts. Required to pay at least the original Medicare rate to out of network providers. 711 October 1 March 31 8 am 8 pm EST 7 days a week April 1 September 30 8 am 8 pm EST Monday Friday.
You pay less if you use doctors hospitals and other health care providers that belong to the plans Network. FOR OUT OF NETWORK PROVIDERS TERMS AND CONDITIONS EFFECTIVE JANUARY 1 2021 These Medicare Advantage Primary Care Physician Incentive Program For Out Of Network Providers¹ Terms and Conditions Terms and Conditions govern the Medicare Advantage Primary Care Physician Incentive MA-PCPi Program. Do all Medicare Advantage plans have Medicare doctor networks.
Out-of-Network coverage rules Bright Health plans are Medicare Advantage plans with a network of doctors hospitals pharmacies and other providers. Medicare preferred provider organizations PPO is one type of Medicare Advantage Medicare Part C plan. The average out-of-pocket limit for in-network services in 2019 Medicare Advantage plans was 5059.
Understand Medicare Advantage MA plan payment obligations to out-of-network providers. Health Maintenance Organizations and Special Needs Plans have stricter regulations on networks. In an HMO plan you generally must get.
Health Net is contracted with Medicare for HMO HMO C-SNP HMO D-SNP and PPO plans and with some state Medicaid programs. In most cases if you choose to see an out-of-network OON provider services will not be covered by your plan and you will be responsible for the full cost of that service. PPO Plans have network doctors other health care providers and hospitals.
Call Member Services at 1-888-445-8913. Providers who have agreed to treat you. When these situations arise providers are often confused.
You must have plan authorization prior to seeking care from an out-of-network provider for services to be covered. You must use plan providers except in emergency situations. You will pay the same for authorized out-of-network services as you would pay if you got the care from a network.
When you see an in-network provider you keep your out-of-pocket costs down. If you join a PFFS plan that doesnt have a network you can go to any Medicare-approved doctor other health care provider or hospital that accepts. Customer Identification Cards provide high-level productnetwork information and.
This document is a general outline of Medicare payments as of the above date and as such does not contain many of the payment details. If you use and out-of-network provider your share of the costs for covered services may be higher. Enrollment in Health Net depends on contract renewal.
When you chose a Bright HealthCare Medicare Advantage plan you were granted access to an extensive network of Care Partner providers. The basic Medicare Advantage out-of-network payment rule is that health care providers who treat Medicare Advantage enrollees on an out-of-network basis must accept as payment in full amounts the provider would have collected if the patient were enrolled in original Medicare. Costs that usually count toward your out-of-pocket maximum include.
Medicare PPO plans have a list of in. If you use providers that are not in our. There are four main types of Medicare Advantage plans which handle networks differently.
If your primary care provider determines that you need Medicare-required medical care that is not available within our network your primary care provider will obtain plan authorization for you to see an out-of-network provider. At the most basic level when a Medicare Advantage HMO member willingly seeks care from an out-of-network provider the member assumes full liability for payment.
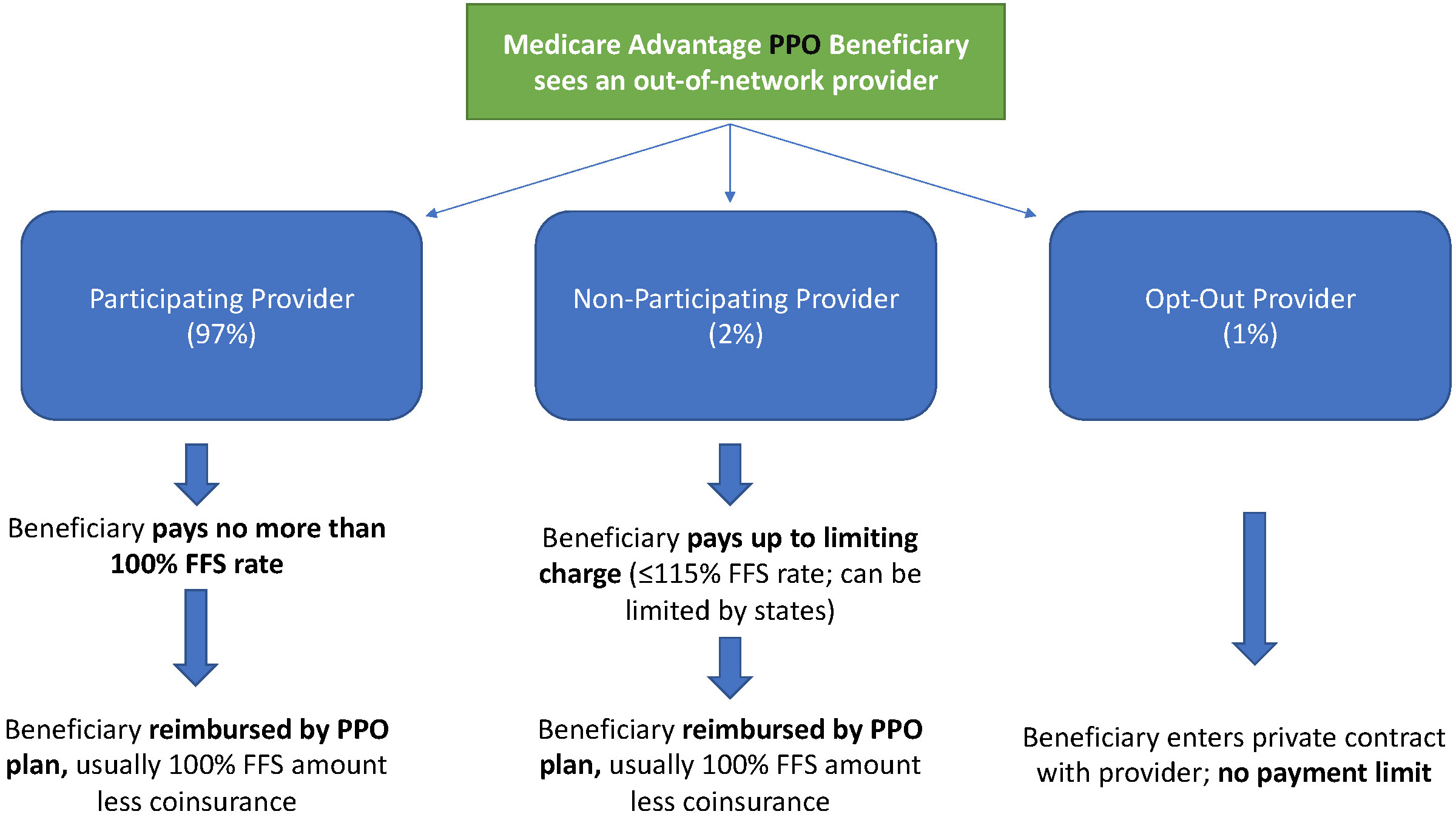 Out Of Network Payments In Medicare Advantage The Incidental Economist
Out Of Network Payments In Medicare Advantage The Incidental Economist
 Is A Medicare Advantage Plan Right For You Aetna Medicare
Is A Medicare Advantage Plan Right For You Aetna Medicare
Medicare Supplement Vs Advantage Plan Which Is Right For You
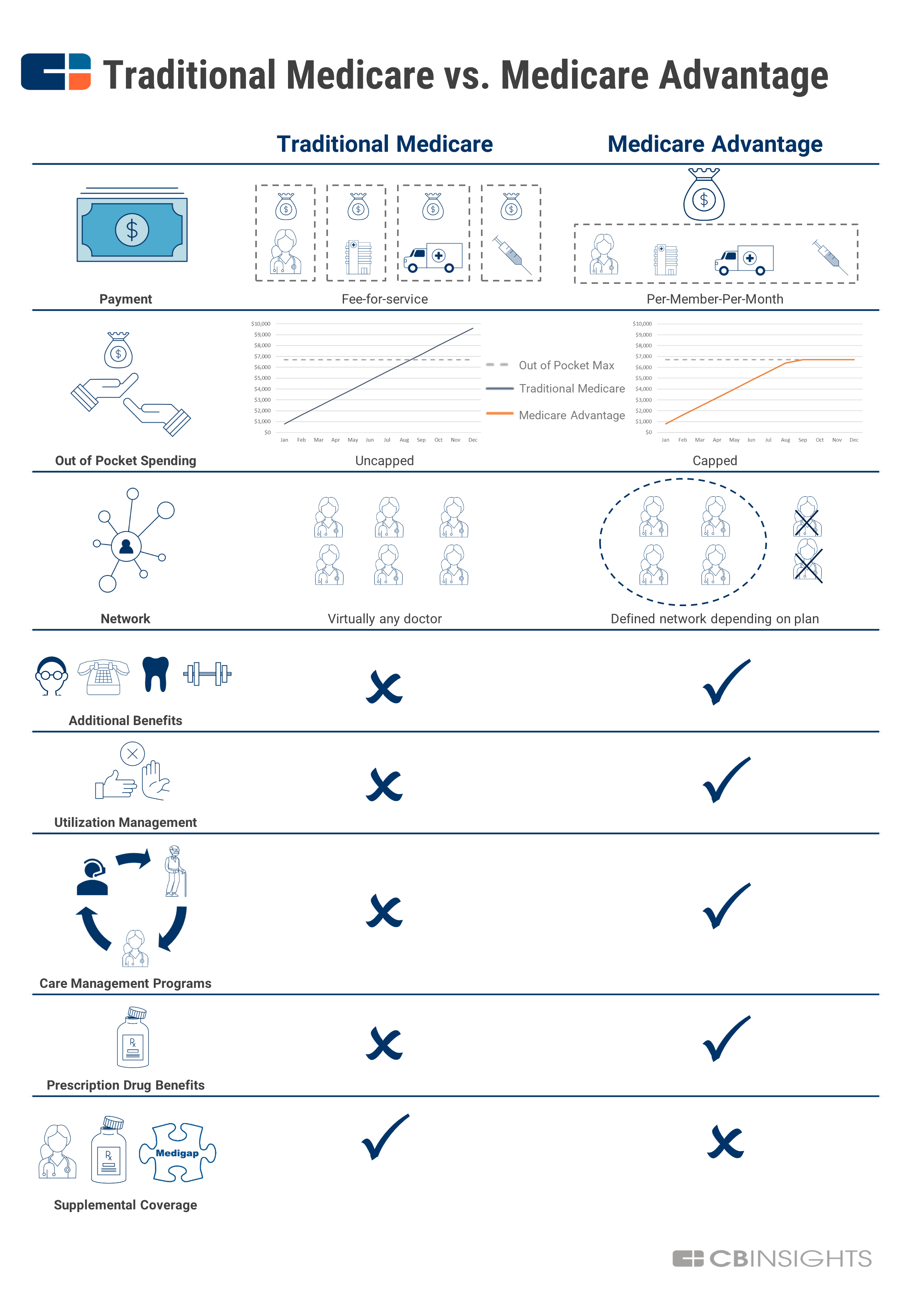
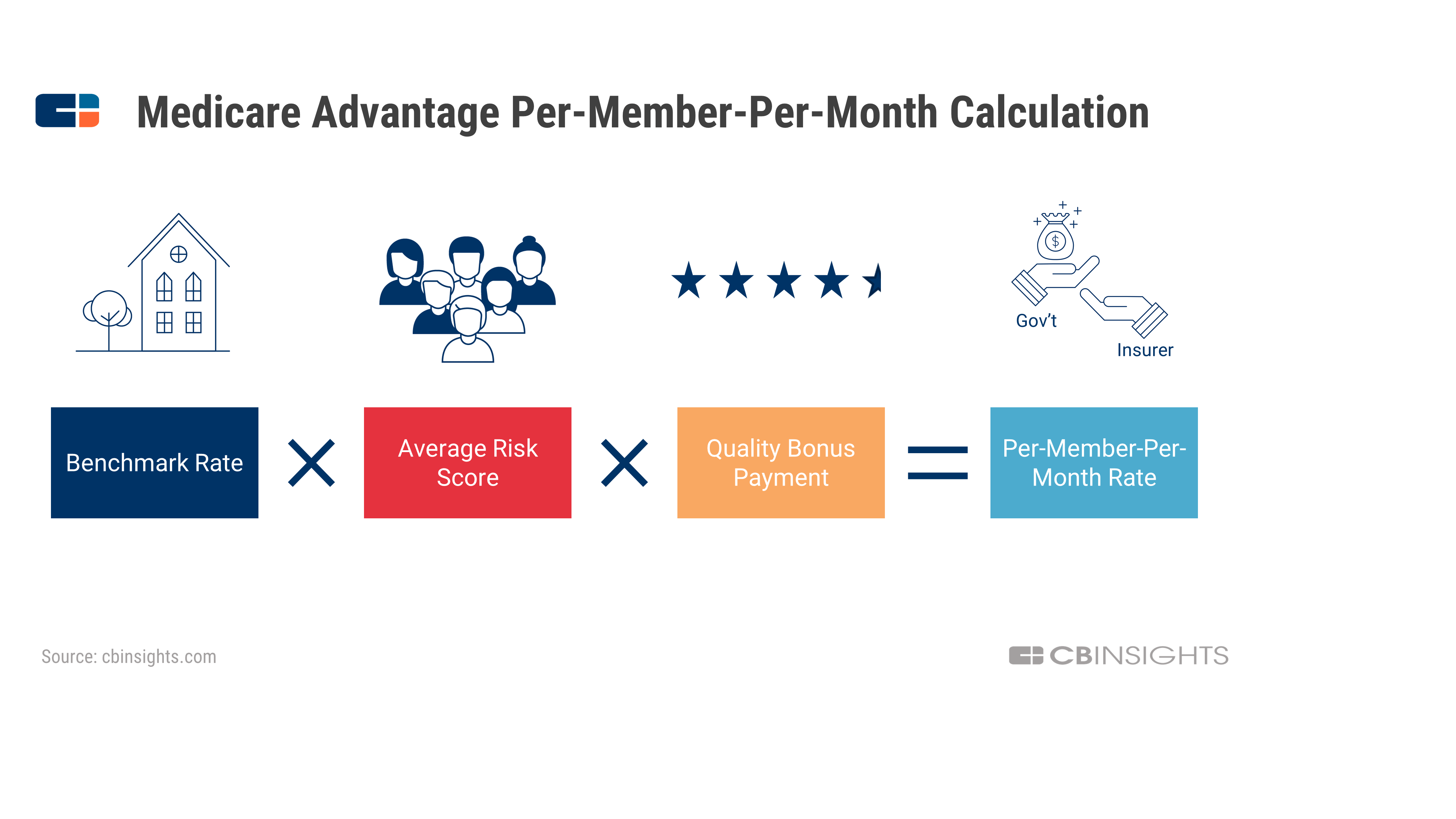
 A Simple Guide To Medicare Advantage And Why It S Taking Off Now Cb Insights Research
A Simple Guide To Medicare Advantage And Why It S Taking Off Now Cb Insights Research
 Original Medicare Vs Medicare Advantage 2020 Boomer Benefits
Original Medicare Vs Medicare Advantage 2020 Boomer Benefits
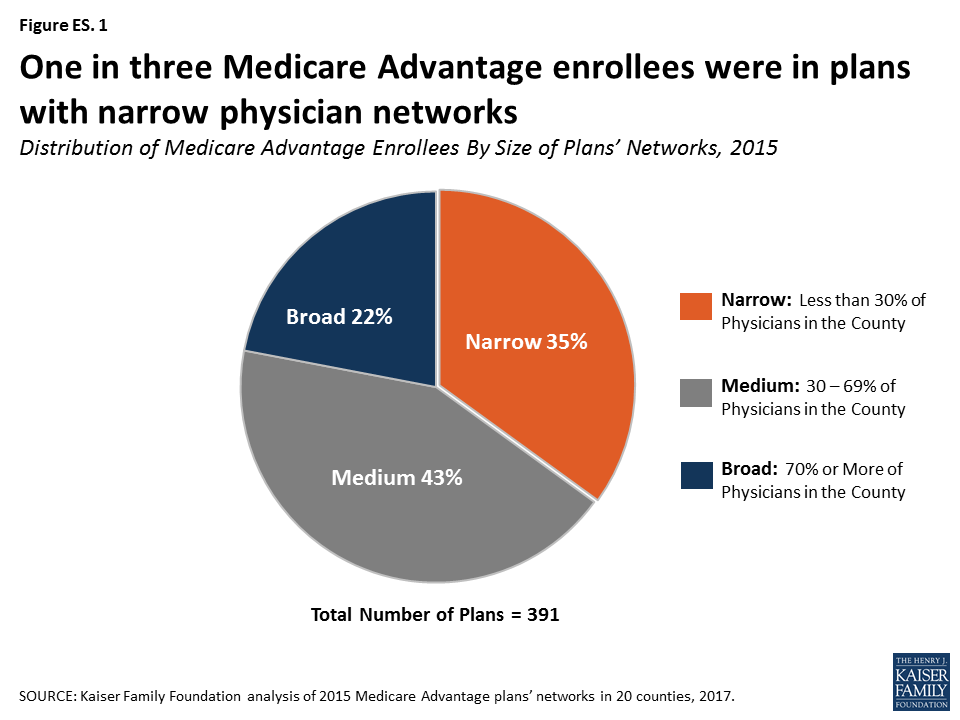 Medicare Advantage How Robust Are Plans Physician Networks Kff
Medicare Advantage How Robust Are Plans Physician Networks Kff
 Medicare Advantage Vs Medicare Supplement Insurance Plans El Aguila News
Medicare Advantage Vs Medicare Supplement Insurance Plans El Aguila News
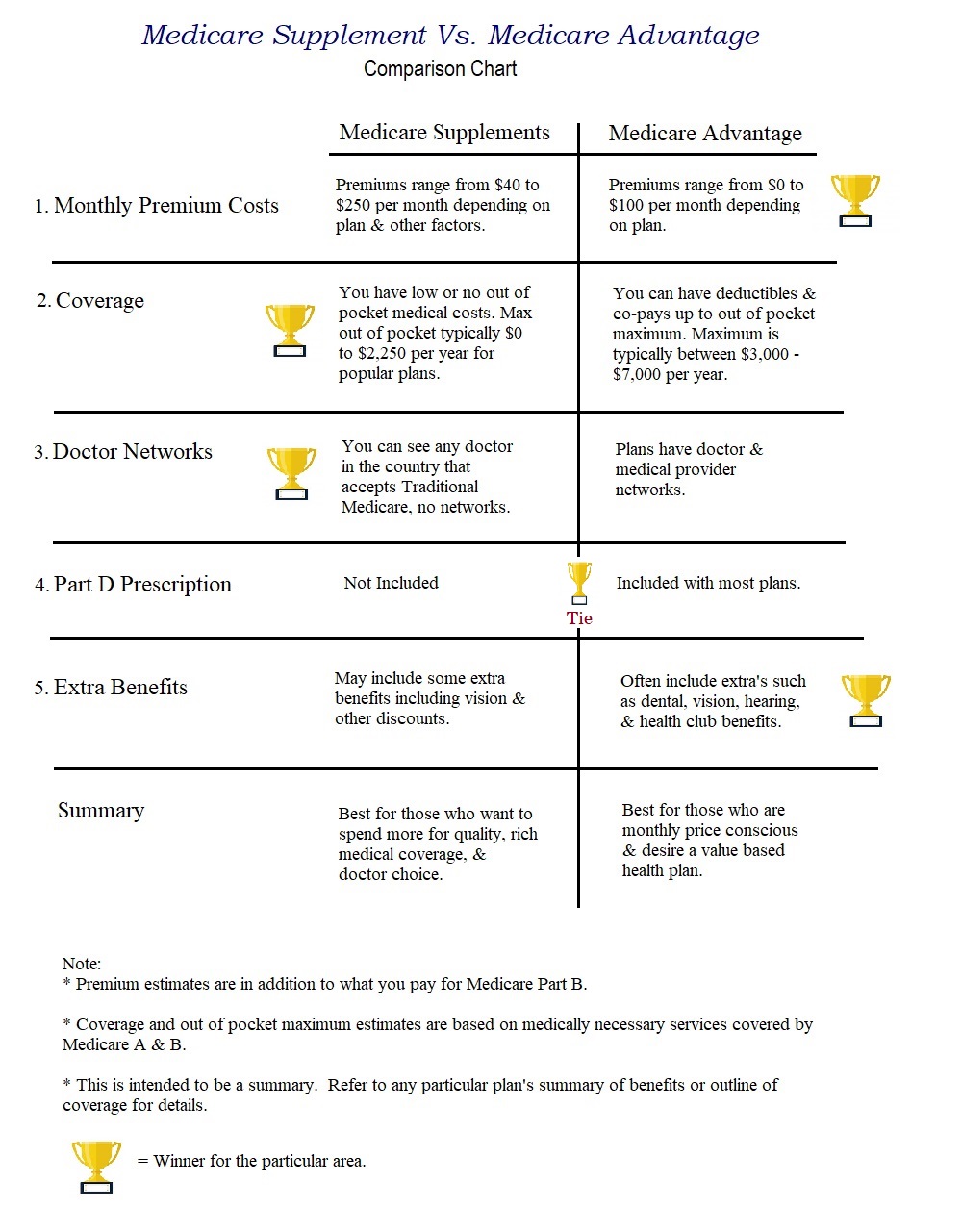 5 Key Areas For Comparing Medicare Supplements Vs Medicare Advantage
5 Key Areas For Comparing Medicare Supplements Vs Medicare Advantage
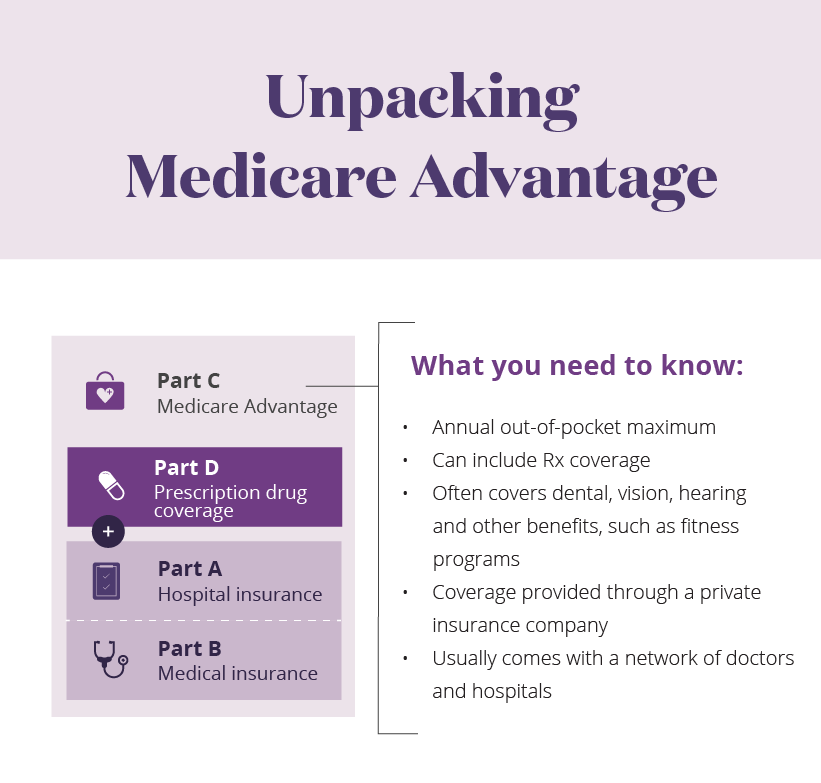
 Medicare Advantage Part C Senior Select Medicare Solutions
Medicare Advantage Part C Senior Select Medicare Solutions
 How To Choose The Best Medicare Advantage Plan In 2021
How To Choose The Best Medicare Advantage Plan In 2021
 Medicare Advantage Plans Hmo And Ppo Abc Medicare Plans
Medicare Advantage Plans Hmo And Ppo Abc Medicare Plans
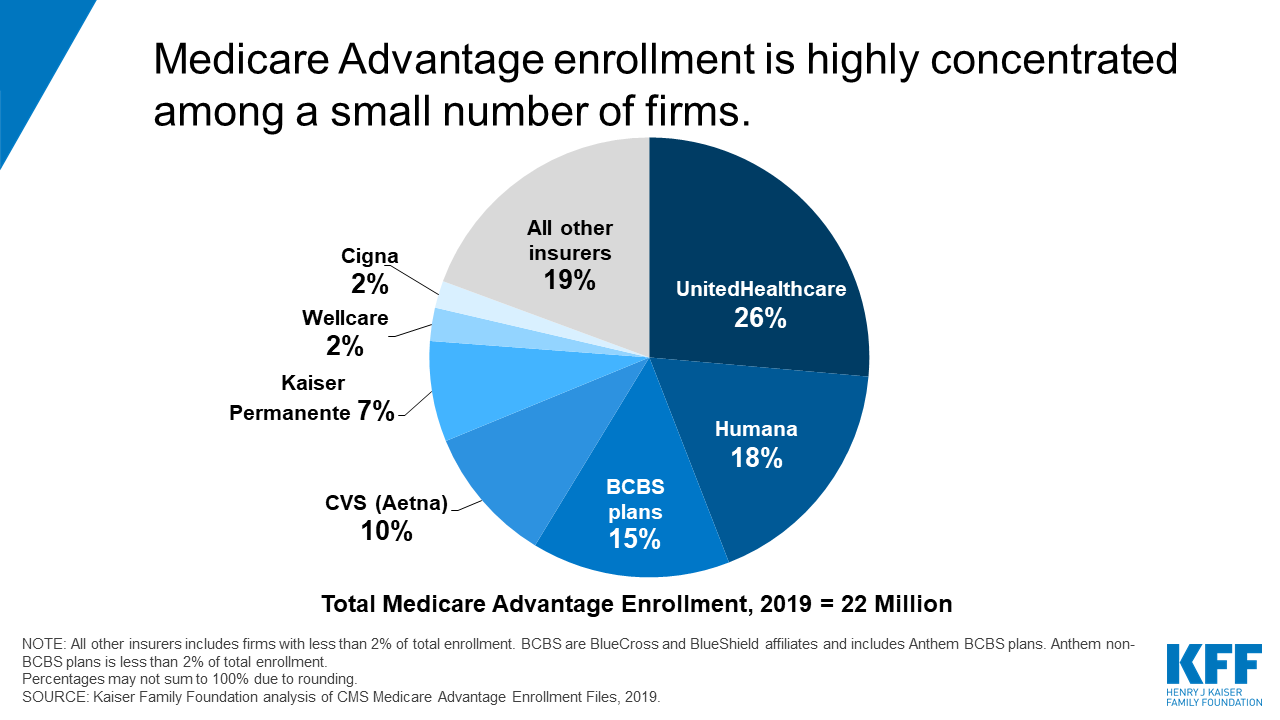 A Dozen Facts About Medicare Advantage In 2019 Kff
A Dozen Facts About Medicare Advantage In 2019 Kff
 A Dozen Facts About Medicare Advantage In 2019 Data Note 9314 Kff
A Dozen Facts About Medicare Advantage In 2019 Data Note 9314 Kff
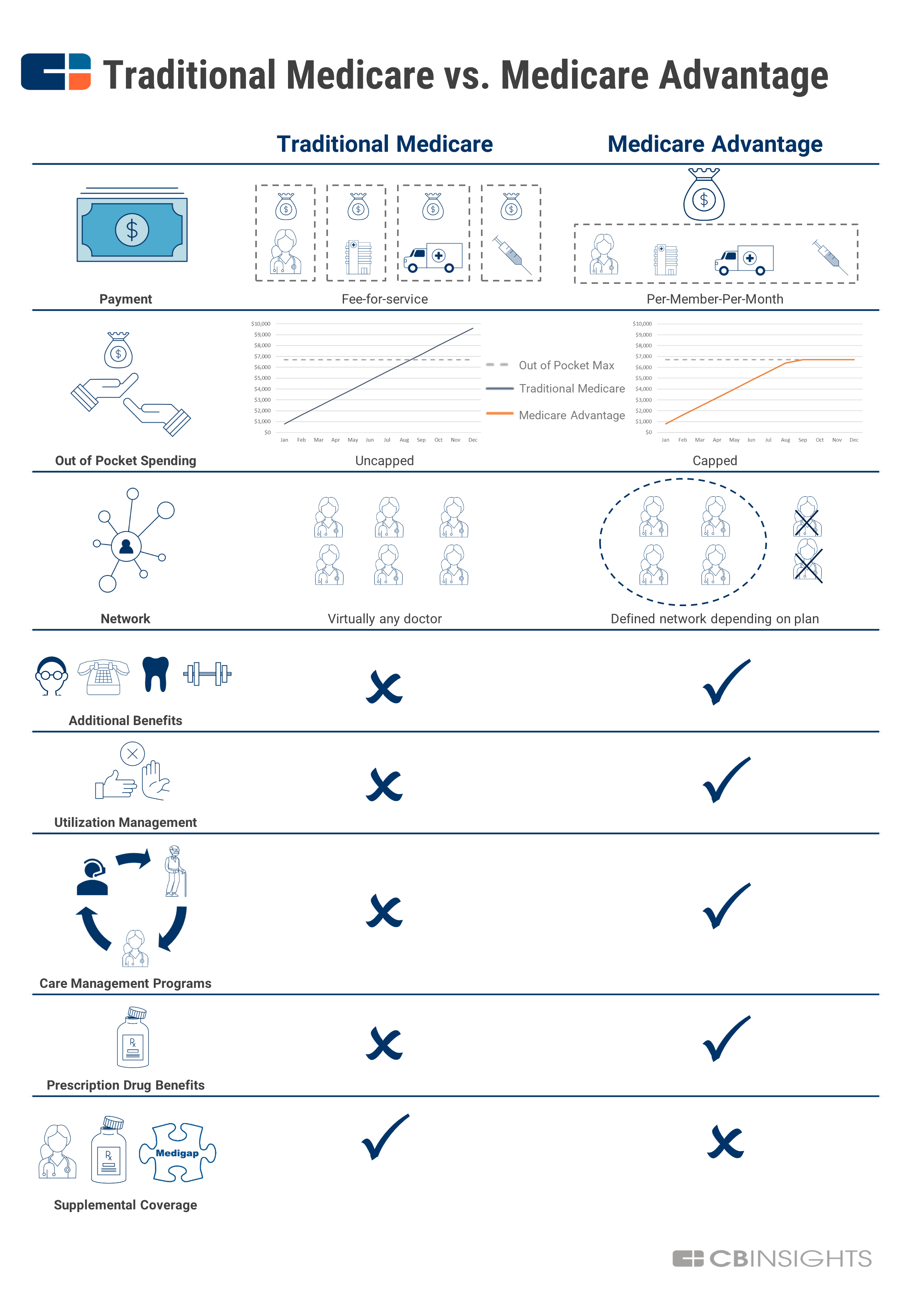
 A Simple Guide To Medicare Advantage And Why It S Taking Off Now Cb Insights Research
A Simple Guide To Medicare Advantage And Why It S Taking Off Now Cb Insights Research
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment