Featured
- Get link
- X
- Other Apps
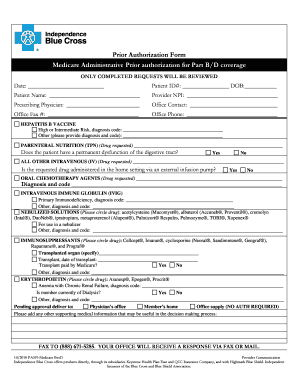
Independence Bcbs Prior Authorization Form
Blue Advantage Physician Drug Authorization Request Form. Independence Blue Cross is a subsidiary of Independence Health Group Inc.
 Fillable Online Direct Ship Injectables Request Form Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Direct Ship Injectables Request Form Independence Blue Cross Fax Email Print Pdffiller
PRIOR AUTHORIZATION requests may require supporting information.
Independence bcbs prior authorization form. However if you would like to submit a request for preauthorization after contacting PRS you may submit a written request by completing this form. As the leading specialty benefits management partner for todays health care organizations we help improve the quality of care and reduce costs for todays most complex tests and treatments. Use the ProviderPortal SM to accelerate your advanced imaging requests and get a.
REQUEST FOR EXPEDITED REVIEW. Authorizations Any provider or third-party agency who contacts the health plan to obtain eligibility request claims status question a claim payment or request an authorization will be directed to use the self-service options on NaviNet. Implant Reimbursement Request Form.
HIPAA Personal Representative Request Form appoints another person as members personal representative. A fast easy way to access AIM Specialty Health. Obtaining a prior authorization helps us pay claims faster with no denied charges or unexpected costs to our members.
Behavioral Health Substance Abuse Continued Stay Review Form. The approval criteria were developed and endorsed by the Pharmacy and Therapeutics Committee and are based on information from the US. Urgentemergency admissions do not require prior authorization.
To 900 pm Eastern Monday through Friday. Once notified of admission medical information is applied against InterQual. 2021 Independence Blue Cross.
At AIM Specialty Health AIM its our mission to promote appropriate safe and affordable health care. Prior Authorization Procedure Codes List for ASO Plans Effective 01012021 - 03312021 Additional codes were added on 12212020 due to AMA code updates AIM Specialty Health AIM is an operating subsidiary of Anthem and an independent medical benefits management company that provides utilization management services for Blue Cross and Blue. Medical policy precertification and preauthorization router.
Please see our Notice of Privacy Practices for more information. If you need preauthorization contact eviCore in one of three ways. AUTHORIZATION REQUEST FORM This form is for authorization of prescription drug benefits only and must be COMPLETELY filled out.
Form Title Networks Expedited Pre-service Clinical Appeal Form. Blue Cross Blue Shield of Michigan Request for Preauthorization Form. Blue Advantage Drug Prior Authorization.
Independence Blue Cross is a subsidiary of Independence. 3 Provider Self -Service Requirements Self-service requirements continued. Medicaid Claims Inquiry or Dispute Request Form.
Call 1-888-233-8158 from 800 am. Independence Blue Cross will not disclose any personal information to outside persons or entities unless we have written consent or unless authorized by law. Most preauthorization requests can be resolved by contacting Provider Relations and Servicing or PRS and requesting member benefits.
Behavioral Health Substance Abuse Certification. An Issuer may also provide an electronic version of this form on its website that you can complete and submit electronically through the issuers portal to request prior authorization of a health care service. Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts.
Supporting Information for an Exception Request or Prior Authorization FORMULARY and TIERING EXCEPTION requests cannot be processed without a prescribers supporting statement. Independent licensees of the Blue Cross and Blue Shield Association serving the health insurance needs of Philadelphia and southeastern Pennsylvania. Medicaid only BCCHP and MMAI Medicaid Service Authorization Dispute Resolution Request Form.
Basically you may need additional approval from your health plan before you receive certain tests procedures or medications. Use this form to request authorization by fax or mail when a n issuer requires prior authorization of a health care service. The Provider Engagement Analytics Reporting PEAR portal is a single point of entry for participating providers to easily access tools to help manage the clinical and financial information specific to their provider organization and to obtain plan information to care for their patients.
This may also be called preapproval pre-authorization or prior authorization. Behavioral Health Case Management Prescreening. Authorization for Disclosure of Mental Health Clinical Information.
GENERAL INFORMATION Patient Name Request Type please check one Prior Authorization Step Therapy Exception Request for Quantity Limit Exception City Appeal Mandatory Generic Exception Request for Non-Formulary Exception. By checking this box and signing below I certify. HIPAA Authorization for Disclosure of Health Information authorizes Independence Blue Cross Independence to release members health information.
To ensure your privacy all information will be sent via a secure connection. Download a form from the Forms Resources section of the Evicore website and fax it to 1-888-693-3210. In a busy practice like yours you need to deliver quality appropriate care efficiently to your patients.
Some services require prior authorization preauthorization before they are performed. Medicaid only BCCHP and MMAI. For members who have prescription drug coverage through Independence Blue Cross Independence prior authorization is required for certain prescribed formulary drugs in order for such drugs to be covered.
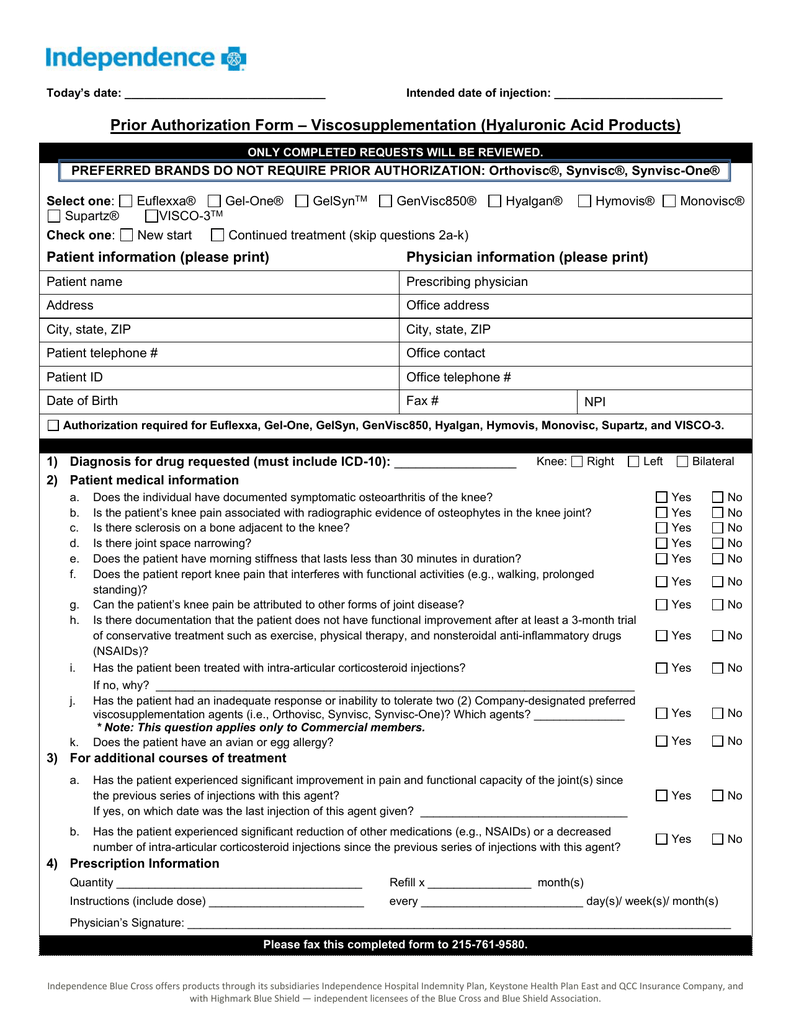 Prior Authorization Form Viscosupplementation Hyaluronic Acid
Prior Authorization Form Viscosupplementation Hyaluronic Acid
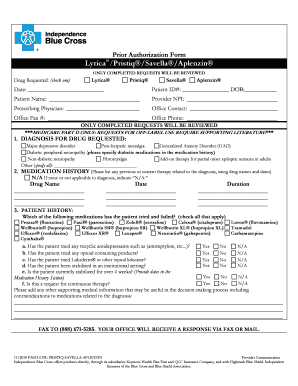
 Prior Authorization Form Lyrica Authorization Form Lyrica Microsoft Word Ibc Author C62sz64 Created Date 10 25 2010 3 33 57 Pm Pdf Document
Prior Authorization Form Lyrica Authorization Form Lyrica Microsoft Word Ibc Author C62sz64 Created Date 10 25 2010 3 33 57 Pm Pdf Document
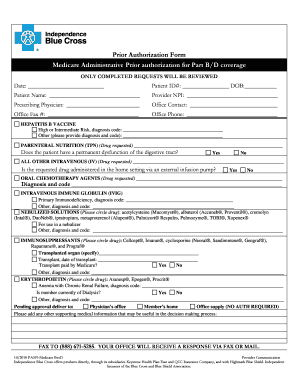
 Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Https Www Ibx Com Documents 35221 56677 Prior Auth Botulinum Toxins Pdf 99b5b638 Fc7c 290b Ab03 58c7a997ef40 T 1580924446000
 Fillable Online Independence Blue Cross Viscosupplementation Prior Authorization Form Independence Blue Cross Viscosupplementation Prior Authorization Form Fax Email Print Pdffiller
Fillable Online Independence Blue Cross Viscosupplementation Prior Authorization Form Independence Blue Cross Viscosupplementation Prior Authorization Form Fax Email Print Pdffiller
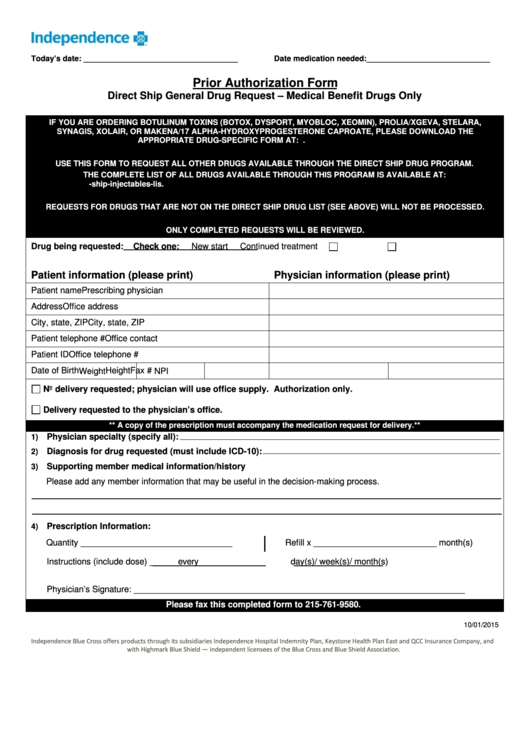 Prior Authorization Form Independence Blue Cross Printable Pdf Download
Prior Authorization Form Independence Blue Cross Printable Pdf Download
 Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Https Www Ibx Com Documents 35221 56677 Prior Auth Makena Pdf 08bf7ea6 Baa2 Bf95 0587 20c06ca3398f T 1580924446433
Https Ibx Com Pdfs Providers Pharmacy Information Prior Authorization Ibc Synvisc Pdf
 Bcbs Prior Auth Forms To Print Fill Online Printable Fillable Blank Pdffiller
Bcbs Prior Auth Forms To Print Fill Online Printable Fillable Blank Pdffiller
 Independence Administrators Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Independence Administrators Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
 Fillable Online Prior Authorization Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Prior Authorization Independence Blue Cross Fax Email Print Pdffiller
Https Www Ibx Com Documents 35221 56677 Prior Auth Prolia Xgeva Pdf 77e8577f Ec58 32b6 67a2 0b4eff40815c T 1580924446700
 Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Independence Blue Cross Fax Email Print Pdffiller
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment