Featured
- Get link
- X
- Other Apps
Bcbs Federal Precertification
These services must meet FEP medical policies which can be accessed at. Drugs on the formulary are assigned to a tier.
Https Www Evicore Com Media Files Evicore Microsites Implementation Blue Cross Blue Shield Bcbs Az All Program Overview Provider Orientation Pdf
Precertification is required for many services including the following outpatient hospital benefits physician benefits and other covered services.
Bcbs federal precertification. Service Benefit Plan Coverage for Federal Employees continued Claims Filing Refer to Section F for the detailed instructions on claims filing. Services that require precertification As of July 1 2020 this list applies to all Independence Blue Cross HMO PPO and POS products including Flex products. Precertification is not a guarantee of payment.
For more information call 877-342-5258 option 3. Federal Employee Standard and Basic Option Beneˇit Plans The Federal Employee Standard and Basic Option Benefit Plans FEP require precertification for the following services. Precertification is our assessment of your patients symptoms and your proposed treatment plan in advance of care.
Precertification BCBSAZ Members-Precert Code Lists. To complete a precertification medical records might be required. Some employer groups have opted out of the eviCore.
Provider Preauthorization and Precertification Requirements - Blue Cross PPO and Medicare Plus Blue SM PPO PDF Northwood DMEPOS Management Program FAQ PDF Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts. Prior review prior plan approval prior authorization prospective review or certification is the process Blue Cross NC uses to review the provision of certain behavioral health medical services and medications against health care management guidelines prior to the services being provided. For services outside Alaska or Washington please contact the local Blue plan where the service is provided.
EviCore precertification is required for most BCBSAZ-insured and -administered benefit plans. 1-800-442-4607 Address written claims inquiries to. The list below displays standard precertification requirements for most BCBSAZ members.
Serving Maryland the District of Columbia and portions of Virginia CareFirst BlueCross BlueShield is the shared business name of CareFirst of Maryland Inc. List applies to most BCBSAZ members member ID prefixes XBB XBM XBP Z3J Z4E Z4M Z4P Z4X Z8M Z5M XBN PMA XBC XBD XBK and XBO City of Phoenix. Type of information being requested.
Precertification requirements are subject to change without notice. Below is the list of specific services in these categories that require precertification. This is called prior approval precertification or preauthorization.
For Federal Employee Program FEP precertification requirements please see the separate FEP precertification list. The formulary is a covered drug list. Please select one at a time.
Please see your benefit booklet to determine what services require precertification under your plan. Federal Claims Inquiries For federal claims inquiries contact BCBSTX Federal Customer Service by calling. 63 rows BCBS Federal Phone Number - FEP List Statewise Customer Service.
Certain medical services and treatments need approval before you receive care. See if you need a precertification or check an existing one For additional guidelines read our Provider Preauthorization and Precertification Requirements PDF. Some large employer groups have custom precertification requirements see table of contents to access these lists.
Precertification approval decisions are based on information provided during the request process. Washington DME prior approval form. Its comprised of generic brand name and specialty drugs.
Preauthorization for physicians and professionals. Alaska DME prior approval form. And Group Hospitalization and Medical Services Inc.
We review them to ensure they are medically necessary. To view the out-of-area Blue Plans medical policy or general pre-certificationpre-authorization information please select the type of information requested enter the first three letters of the members identification number on the Blue Cross Blue Shield ID card and click GO. In some situations you need to get your care treatment or prescription drugs approved before we cover them.
To view the out-of-area Blue Plans medical policy or general pre-certificationpre-authorization information please select the type of information requested enter the first three-characters of the members identification number on the Blue Cross Blue Shield ID card and click GO. In the District of Columbia and Maryland CareFirst MedPlus is the business name of First Care Inc. EviCore precertification is NOT required for.
This applies to services performed on an elective non-emergency basis. Washington prior approval form. EviCore precertification program information is highlighted in yellow.
Our 2021 precertification code list spreadsheet now includes a tab for each the following code lists. Federal Employee Program FEP members BlueCard out-of-area members from other Blue plans Corporate Health Services CHS employee group members. BCBSTX FEP Customer Service PO.
For durable medical equipment DME prior approvals.
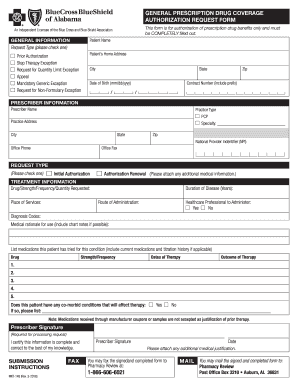 2016 2021 Form Al Bcbs Mkt 148 Fill Online Printable Fillable Blank Pdffiller
2016 2021 Form Al Bcbs Mkt 148 Fill Online Printable Fillable Blank Pdffiller
Https Www Bcbstx Com Provider Pdf Bcf Federal Employee Pdf
 Bcbs Federal Provider Appeal Form Best Of File Plaint Blue Shield Pharmacy Prior Authorization Models Form Ideas
Bcbs Federal Provider Appeal Form Best Of File Plaint Blue Shield Pharmacy Prior Authorization Models Form Ideas
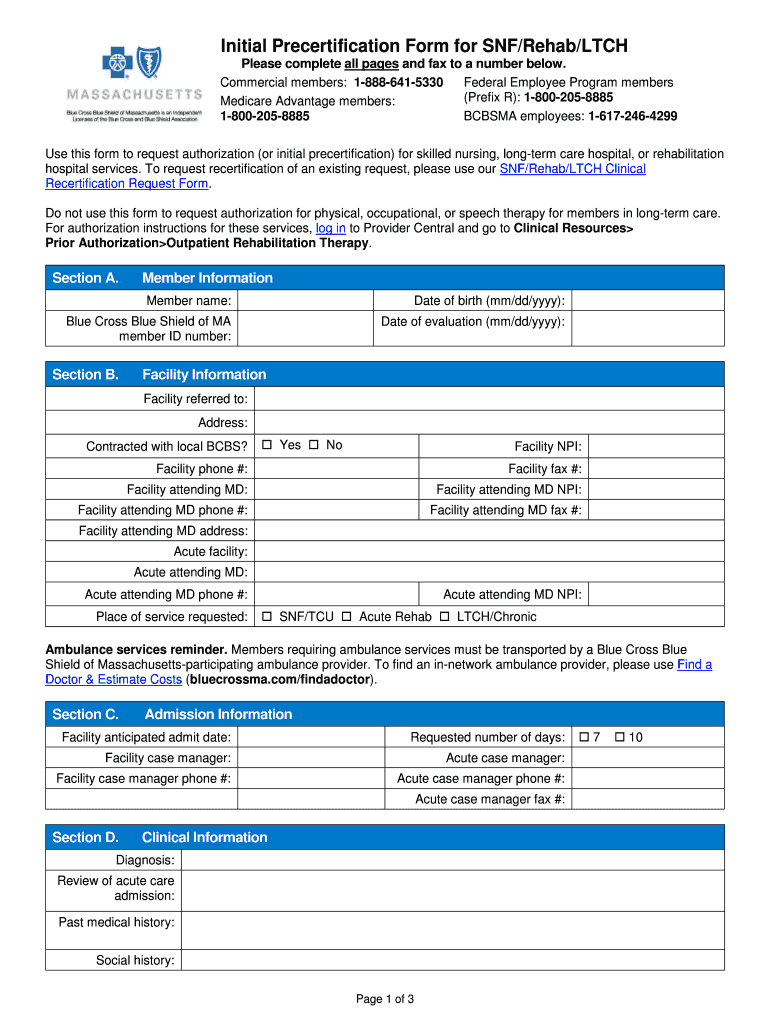 Ma Blue Cross Initial Precertification Form For Snf Rehab Ltch 2019 2021 Fill And Sign Printable Template Online Us Legal Forms
Ma Blue Cross Initial Precertification Form For Snf Rehab Ltch 2019 2021 Fill And Sign Printable Template Online Us Legal Forms
Https Www Bcbstx Com Provider Pdf Bcf Federal Employee Pdf
Https Www Blueshieldca Com Bsca Bsc Public Common Portalcomponents Provider Streamdocumentservlet Filename Prv Fep Medical Injectable Drug Pdf
Https Www Bcbsvt Com Sites Default Files 2020 02 2020 Fep Blue Focus Pa List 12 18 19 Pdf
 Bcbs Federal Provider Appeal Form Unique Fep Prior Authorization Form A Models Form Ideas
Bcbs Federal Provider Appeal Form Unique Fep Prior Authorization Form A Models Form Ideas
Https Www Ibx Com Pdfs Providers Policies Guidelines Preapproval Fep Precert Pdf
Https Www Bcbstx Com Provider Pdf Bcf Federal Employee Pdf
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
Https Bluecrosscamedicarerx Com Ca Provider F1 S0 T0 Pw E237667 Pdf Refer Provider
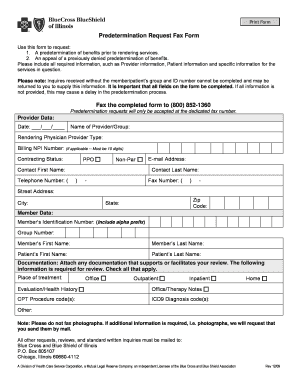 Bcbs Florida Predetermination Form Fill Online Printable Fillable Blank Pdffiller
Bcbs Florida Predetermination Form Fill Online Printable Fillable Blank Pdffiller
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment