Featured
Apply For Cobra
If you are newly eligible under the relief bill your employer is required to notify you by May. MS Word PDF.
Https Www Nh Gov Insurance Consumers Documents Federal Cobra Nh State Continuation Coverage Pdf
1 Your current health plan must be subject to the COBRA law.

Apply for cobra. Additionally the employees must have been employed for more than 50 of the business days the previous year. Period is also available when you reach the end of your maximum COBRA coverage period. You must be considered a qualified beneficiary of your current health plan.
Qualified beneficiaries then have 60 days to elect coverage. Federal COBRA is a federal law that lets you keep your group health plan when your job ends or your hours are cut. If youre eligible for COBRA because of a reduction in the hours you work or you involuntarily lost your job you may qualify for help paying for your COBRA premiums called premium assistance from April 1 2021 through September 30 2021 under the American Rescue Plan Act of 2021 based on how long your COBRA coverage can last.
Employers must notify qualified beneficiaries about COBRA eligibility within 14 days of a qualifying event. Not all health plans are. According to the Department of Labor to qualify for COBRA you must fall under three conditions to be considered for coverage.
If you have a family health plan not all family members have to enroll in COBRA. COBRA applies to private-sector companies with 20 or more employees as well as state and local governments. Federal COBRA requires continuation coverage be offered to covered employees their spouses former spouses and dependent children.
The applicant person requesting review of a denial of premium assistance may either be the former employee or a member of the employees family who is eligible for COBRA continuation coverage or the COBRA premium assistance through an employment-based health plan. Also as noted above persons who lost coverage due to reduced hours or involuntary termination before April 1 2021 now have a second chance to elect COBRA and request the subsidy. To be eligible for COBRA you must satisfy all three of the following requirements.
Federal COBRA applies to employers and group health plans that cover 20 or more employees. For more information go to. Some states also have mini-COBRA laws that apply to employers with fewer than 20 workers.
The extended deadlines do NOT apply to the COBRA subsidy. COBRA is a federal law that may let you keep your employer Group health plan coverage for a limited time after your employment ends or you lose coverage as a dependent of the covered employee. Also available in Spanish MS Word PDF.
Its also available to employees who didnt opt into COBRA. Individuals receiving the COBRA premium assistance must notify their plans if they become. COBRA covers group health plans only when sponsored by an employer who has at least 20 employees.
How to apply. But if the company goes out of business and closes the health plan then COBRA is not an option. See the section below for more information about mini-COBRA plans.
Per CNBC the 100 subsidy on premiums apply to everyone who already qualifies for COBRA. Each qualified beneficiary can decide independently to elect COBRA coverage or to waive. That means that employers need to provide COBRA notices including information about the subsidy option within 44 days of the COBRA event.
How to enroll in COBRA In general employers have 60 days to notify you of your COBRA eligibility. This is called continuation coverage In general COBRA only applies to employers with 20 or more employees. You likely have access to COBRA if you worked for an employer with more than 20 employees.
Model Notice in Connection with Extended Election Period. You are eligible both if youve left your job voluntarily or have been laid off. The employee and his or her family members may each elect to continue health.
The Consolidated Omnibus Budget Reconciliation Act COBRA gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss reduction in the hours worked transition between jobs death divorce and other. However some states require insurers covering. You may apply for and if eligible enroll in Medicaid coverage at any time.
Learn more about COBRA which allows you to keep health insurance when your job changes unexpectedly. Model General Notice and COBRA Continuation Coverage Election Notice. COBRA Insurance Knowledge Base General insurance information provided on COBRA Insurance Website is not intended to substitute for informed professional medical psychological tax legal investment accounting governmental or other professional advice.
 Top 10 Cobra Mistakes And How To Avoid Them
Top 10 Cobra Mistakes And How To Avoid Them
 How To Sign Up For Cobra Insurance 8 Steps With Pictures
How To Sign Up For Cobra Insurance 8 Steps With Pictures

 Top 10 Cobra Mistakes And How To Avoid Them
Top 10 Cobra Mistakes And How To Avoid Them
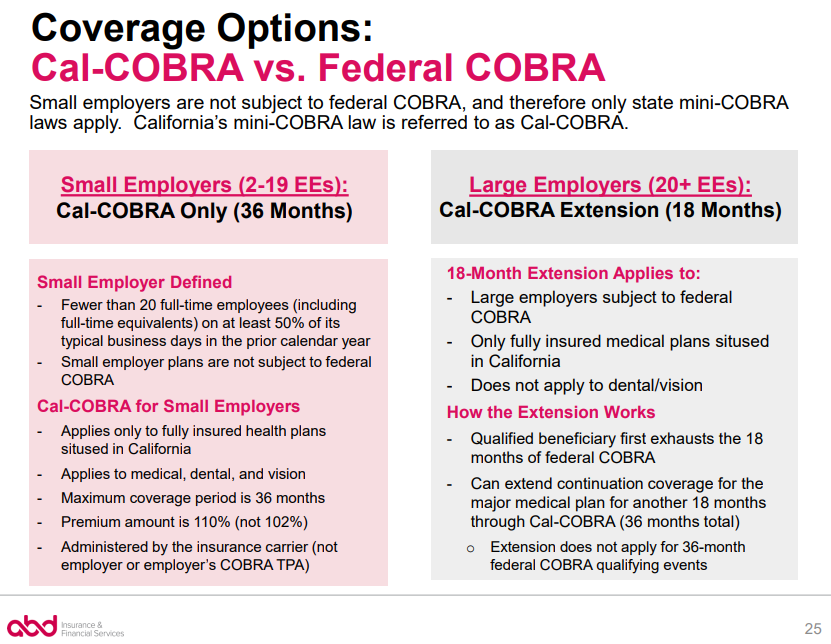 Cobra Small Employer Exception Abd Insurance Financial Services
Cobra Small Employer Exception Abd Insurance Financial Services
 6 Reasons Cobra Coverage Ends Early Bri Benefit Resource
6 Reasons Cobra Coverage Ends Early Bri Benefit Resource
 How To Sign Up For Cobra Insurance 8 Steps With Pictures
How To Sign Up For Cobra Insurance 8 Steps With Pictures
 Extreme Einsatze Was Cobra Beamte Leisten Mussen News At
Extreme Einsatze Was Cobra Beamte Leisten Mussen News At
 Cobra Health Insurance Coverage Benefits Cost And How To Apply
Cobra Health Insurance Coverage Benefits Cost And How To Apply
 Health Insurance And Cobra Austin Asset Management Austin Asset
Health Insurance And Cobra Austin Asset Management Austin Asset
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps


Comments
Post a Comment