Featured
- Get link
- X
- Other Apps
What Is Split Billing In Healthcare
Payment by or to a physician or health care institution solely for referral of a patient is fee splitting and is unethical. In most parts of the world the practice is considered unethical and unacceptable hence fee splitting.
 Understanding Split Billing For Post Op Care
Understanding Split Billing For Post Op Care
Any payment of any kind from any source for referring a patient other than distributions of a health care organizations revenues as permitted by law.

What is split billing in healthcare. One is sent to the medical scheme listing the medical scheme tariff amount and another to the member or patient. In the United States balance billing usually happens when you get care from a doctor or hospital that isnt part of your health insurance companys provider network or doesnt accept Medicare or Medicaid rates as payment in full. Technical charges can cover the facility overhead materials medications nurses support staff etc.
The fiscal year is any 12 consecutive months chosen to be the official accounting period by a business or organization. Split-billing occurs when a medical supplier provides two accounts for the same service. Fee splitting prohibitions are aimed primarily at situations where a healthcare professional in order to generate patient referrals from other licensed or unlicensed persons splits part of the professional fee earned from treating the referred patient with the source of the referral.
Physicians may not accept. The Admission Date FL 12 is the date the patient was admitted as an inpatient to the facility or indicates the start of care date for home health and hospice. August 02 2016 - Medical billing is the backbone of healthcare revenue cycle management but many providers experience significant challenges with efficiently and accurately billing patients and payers for services they perform.
The guidance for billing in these two settings can both be found within the Medicare Claims Processing Manual first of which comes in chapter 1 section 7081. It is reported on all inpatient claims regardless of whether it is an initial interim or final bill. The medical billing process can be a pain point for some providers because it involves an array of healthcare stakeholders and each step to getting paid relies.
This post focuses on a specialty situation Split-Claim Billing that can impact how a claim is billed. The concept of split billing in both the inpatient and outpatient setting is a hot topic amongst providers as of late according to Debbie Mackaman RHIA CHCO regulatory specialist for HCPro Inc. This is essentially the payment of a commission to the referrer with the express intention of ensuring that the referring doctor directs referrals of patients to the payee.
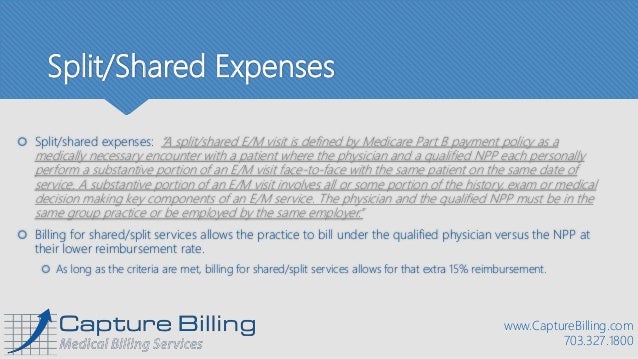
This process is most commonly referred to as split billing. An example of so-called split billing is when the provider performs a physical exam and also discusses the patients chronic pre-existing conditions linking the chronic diagnosis codes to the office visit and the reason for the visit V700 Routine general medical examination at a health care facility to the preventive service. When an EM service is performed in the hospital inpatienthospital outpatient or emergency department and is shared between a physician and a NPP from the same group practice the service may be billed as a splitshared EM service.
Most claims are comprised of two types of charges professional and technical. The member will pay the supplier what they think is a co-payment but the amount paid does not appear on the claim sent to the. Inpatient Split Billing There are times when an inpatient admission may cross over the providers fiscal year end the federal fiscal year end or calendar year end.
Fee splitting in medicine and healthcare. The second claim is submitted with the facility charges and paid by Medicare using the OPPS Hospital Outpatient Prospective Payment System. Professional charges cover the fee of the physician.
Split insurance billing insurancepatient in healthcare practice in QBO. Shared or split visits are one of the important services that medical billing and coding companies help healthcare providers report. In 2002 the Centers for Medicare Medicaid Services CMS issued instructions giving non-physician practitioners NPPs and their supervising physicians increased flexibility for hospital and office billing of evaluation and management EM services.
The admission date and From dates are not required to match. Any payment of any kind from any source. Even though you see the insurance company name first in the customer listing when you invoice within the patient their name shows.
When the payments are combined the payment is generally higher then what the practice could expect to receive as a free-standing facility. Just to reiterate it seems making the insurance company the parent and multiple respective patients as sub-patient works best.
Https Www Docweb Co Za Practice Management General Send 58 Billing Coding Split Billing 20versus 20balance Billing Pdf
 Healthcare Payer Value Chain Key Functional Split And Outsourced Download Scientific Diagram
Healthcare Payer Value Chain Key Functional Split And Outsourced Download Scientific Diagram
 Pdf E Healthcare Billing And Record Management Information System Using Android With Cloud Semantic Scholar
Pdf E Healthcare Billing And Record Management Information System Using Android With Cloud Semantic Scholar
 Medical Supply Store Software Pos Inventory Control Accounting Crm Point Of Sale
Medical Supply Store Software Pos Inventory Control Accounting Crm Point Of Sale
 Sdg Health Price Tag We Have The Numbers How Do We Split The Bill P4h Network
Sdg Health Price Tag We Have The Numbers How Do We Split The Bill P4h Network
 Benefits Of Split Shared Billing Servicemedical Billing And Coding Services
Benefits Of Split Shared Billing Servicemedical Billing And Coding Services
What Is Split Billing And How Do I Use It
 Hospitals May Have To Split Medicines Services Bill For Tax The Economic Times
Hospitals May Have To Split Medicines Services Bill For Tax The Economic Times
 Telehealth And Covid 19 Billing And Coding Resources
Telehealth And Covid 19 Billing And Coding Resources
 What Is Medicare Split Claim Billing How To Do It
What Is Medicare Split Claim Billing How To Do It
 Coding And Billing For Np And Pa Providers In Your Medical Practice
Coding And Billing For Np And Pa Providers In Your Medical Practice
 5 Ways To Avoid Common Medical Claim Errors
5 Ways To Avoid Common Medical Claim Errors
 The Anatomy Of Incident To And Split Shared Billing
The Anatomy Of Incident To And Split Shared Billing
 Hospitals May Have To Split Medicines Services Bill For Tax The Economic Times
Hospitals May Have To Split Medicines Services Bill For Tax The Economic Times
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment