Featured
Is Medicare Primary Or Secondary
When Is Medicare A Secondary Payer. Employer Insurance Medicare By CornerstoneSeniorAdvisors.
 Understanding Medicare Secondary Payer Rules
Understanding Medicare Secondary Payer Rules
We just addressed the fact that Medicare is always the secondary payer of benefits to Non-Group Health Plan insurance and when certain conditions are met the secondary payer to Group Health Plan insurance.
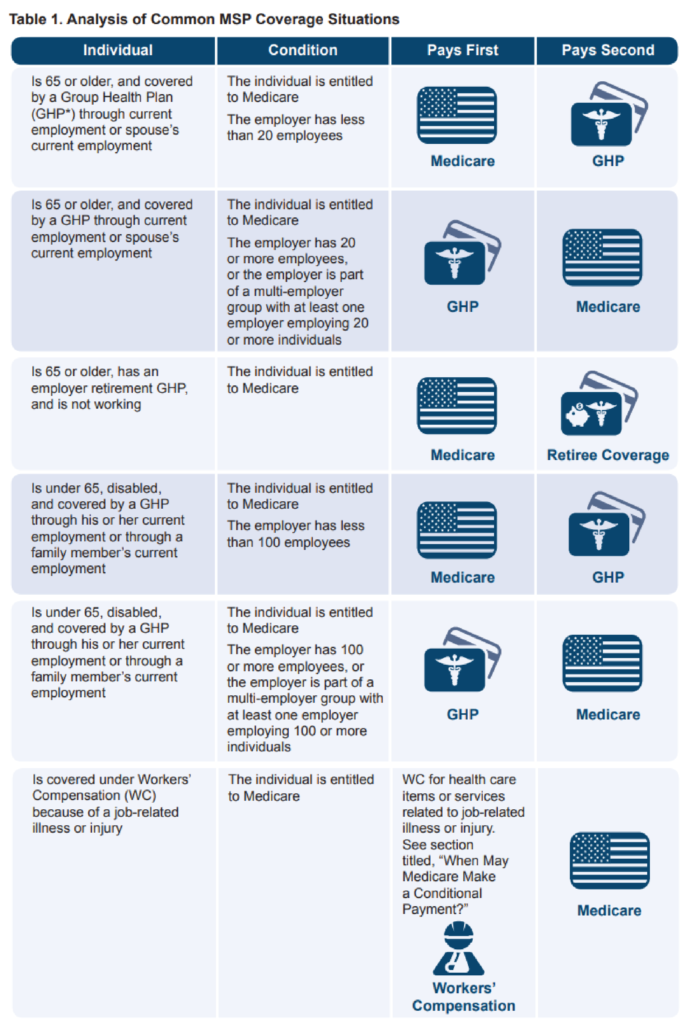
Is medicare primary or secondary. But Medicare becomes the secondary payer if your employer is. Medicare is the secondary payer if the recipient is. Even if an entity believes that it is the secondary payer to Medicare due to state law or the contents of its insurance policy the MSP provisions would apply when billing for services.
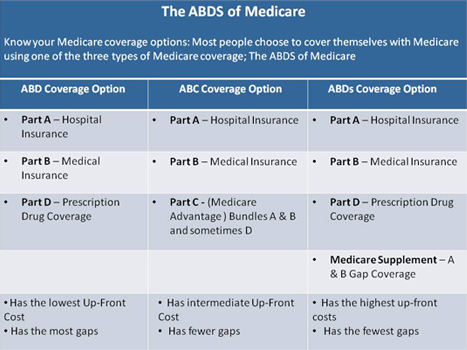
If your employer insurance is the secondary payer you may need to enroll in Medicare Part B before your insurance will pay. With a Medigap policy the supplement is secondary. The secondary payer which may be Medicare may not pay all the uncovered costs.
Mostly Medicare is primary. So can Medicare Advantage be the secondary payer. Medicare is the primary payer when a beneficiary does not have other primary insurance as.
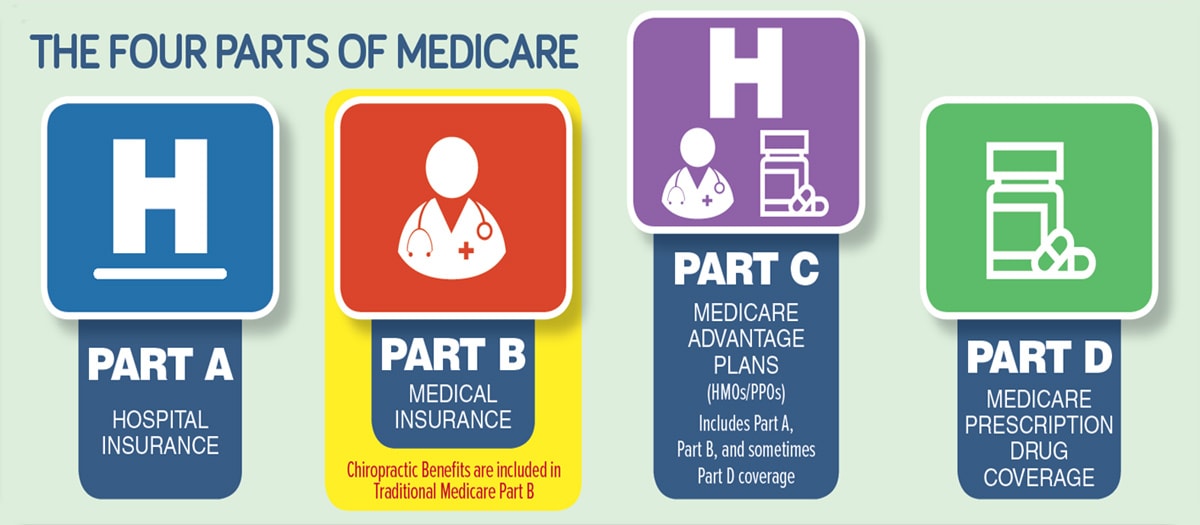
When Medicare is primary and secondary When you have Medicare and another type of insurance Medicare is either your primary or secondary insurer. There are separate rules for individuals who are Medicare-eligible due to End-Stage Renal Disease ESRD. When Medicare is Primary Primary insurance means that it pays first for any healthcare services you receive.
The one that pays second secondary payer only pays if there are costs the primary insurer didnt cover. In situations where Medicare is a secondary payer it will still cover all the same things as a primary payer situationtheyll just be second-in-line for coverage after the primary payer takes care of as much as they can. Medicare will generally be the primary payer and your additional insurance plan will be the secondary payer.
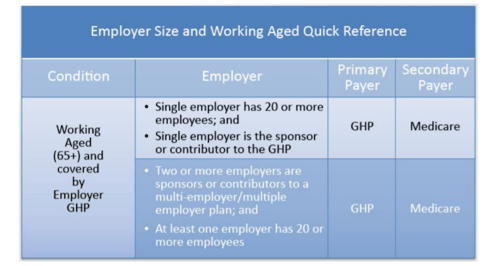
However if you have ESRD and have both a COBRA plan and Medicare then Medicare will be your secondary payer and your COBRA plan will pay first. The primary payer may not cover some things that Medicare does and vice versa so its especially nice to have both sources to cover healthcare costs. Medicare is generally the primary payer if the company you work for has fewer than 20 employees.
If you are over 65 and dont have Medicare due to ESRD End-Stage Renal Disease then Medicare will be your primary payer. In most cases the secondary insurance wont pay unless the primary insurance has first paid its share. If you have a Medicare Advantage plan see below.
When multiple insurance companies are involved one becomes the primary or first to pay and one becomes the secondary paying after the primary has paid its share of the costs. While Medicare usually is the primary insurance there are some instances when Medicare is secondary. Secondary payers can help cover out-of-pocket costs and services Medicare.
If you have a COBRA plan Medicare will pay first under some circumstances. Medicare Secondary Payer MSP is the term generally used when the Medicare program does not have primary payment responsibility - that is when another entity has the responsibility for paying before Medicare. Certainly Medicare can be the primary or the secondary payer depending on the situation.
Medicare pays claims first and then Medigap pays. For patients that have both Medicare and Medicaid and no other insurance Medicare is the primary payer In most cases federal law takes precedence over state laws and private contracts. After the coordination period Medicare pays first and the group health plan pays second.
There are a number of situations when Medicare is primary. Sometimes Medicare is the primary payer and sometimes the secondary payer. When Medicare began in 1966 it was the primary payer for all claims except for those covered by Workers Compensation Federal Black Lung benefits and Veterans.
If Medicare is not aware of other primary insurance Medicare may. Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization with more than 20 employees. When we are talking abo.
Two common instances are. This is often a beneficial relationship to the insured who has extra help paying for costs beyond the. If you have job-based insurance from an employer with 20 or more employees This is the case whether you get insurance through your company or.
The primary insurer is the one that pays the claim first whereas the secondary insurer pays second. If you originally got Medicare due to your age or a disability other than ESRD and your group health plan was your primary payer then it still pays first when you become eligible because of ESRD. Use the table below to learn how Medicare coordinates with other insurances.
Medicare pays second.
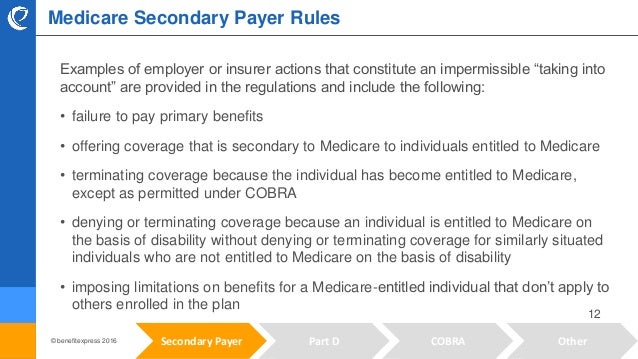
Demystifying The Medicare Secondary Payer Rules
 How To Determine When Medicare Is Primary
How To Determine When Medicare Is Primary
 Know All Types Of Primary Medicare Coverage Kmc University
Know All Types Of Primary Medicare Coverage Kmc University
 What Is Medicare Secondary Payer Ametros
What Is Medicare Secondary Payer Ametros
Https Www Cms Gov Medicare Coordination Of Benefits And Recovery Mandatory Insurer Reporting For Group Health Plans Ghp Training Material Downloads Msp Employer Size For Ghp Arrangements Part 1 Pdf
 Medicare Secondary Payer Employer Size Requirements Abd Insurance Financial Services
Medicare Secondary Payer Employer Size Requirements Abd Insurance Financial Services
 Medicare Minute Medicare Employer Based Coverage Teresa D Mitchell
Medicare Minute Medicare Employer Based Coverage Teresa D Mitchell
Https Www Flexiben Com Files Images Pdfs Mspguidelines Pdf
 Medicare As A Secondary Insurance Customer
Medicare As A Secondary Insurance Customer
 Medicare Rule Review Overview Of Secondary Payers
Medicare Rule Review Overview Of Secondary Payers
 When Is Medicare Primary And When Is It Secondary Boomer Benefits
When Is Medicare Primary And When Is It Secondary Boomer Benefits
 Medicare Secondary Payer Navigating The Trenches
Medicare Secondary Payer Navigating The Trenches
 Infographic Which Is Primary Medicare And Employer Coverage Medicare Rights Center
Infographic Which Is Primary Medicare And Employer Coverage Medicare Rights Center
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps

Comments
Post a Comment