Featured
- Get link
- X
- Other Apps
Priority Health Authorization
This form allows you to choose someone you trust to access your health records. You can also decide how much of your personal health information you want that person to know.
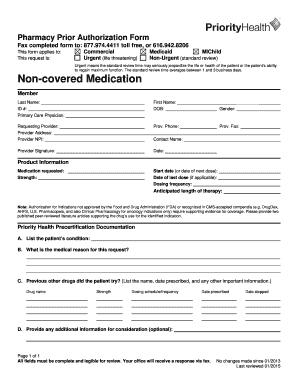
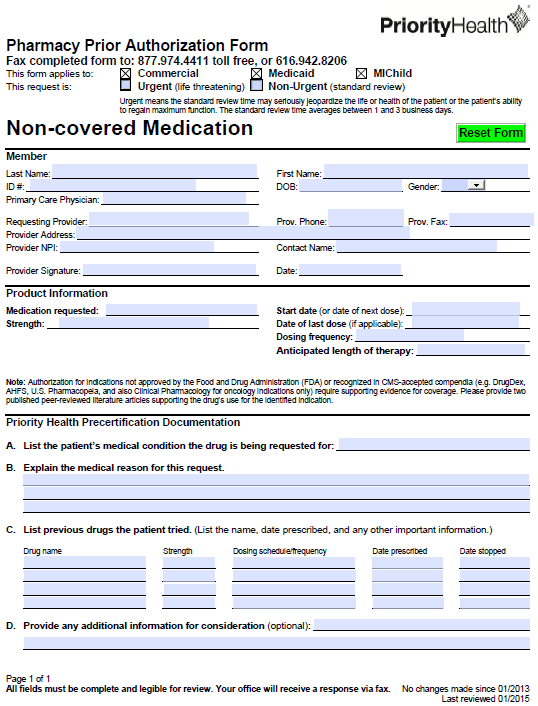
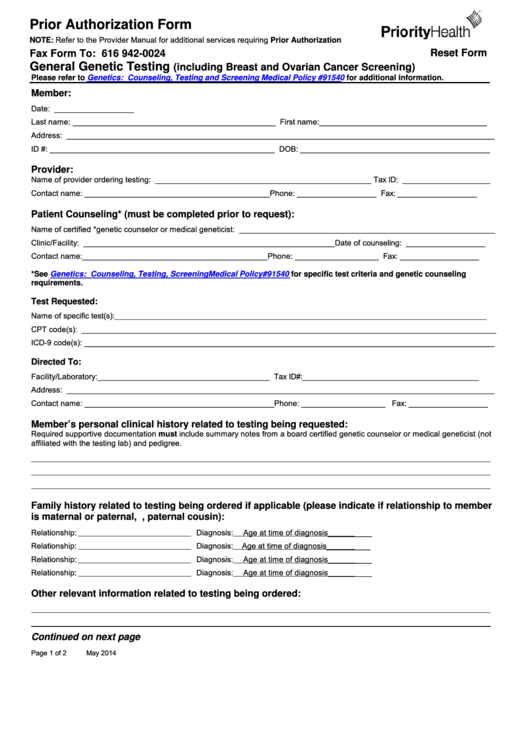 Fillable Prior Authorization Form Priority Health Printable Pdf Download
Fillable Prior Authorization Form Priority Health Printable Pdf Download
410-424 -4894 TransplantBariatric Outpatient Medical.

Priority health authorization. Permission to release health information Stagant. A priority is a way for health pharmacy pre-authorization form plan members to obtain coverage for the non-covered drug. Prescriber means the term as defined in section 17708 of the Public Health Code 1978 PA 368 MCL 33317708.
If you dont get approval Priority Health Medicare may not cover the drug. Prior authorizations also help us understand and review. See if you qualify.
Prior Authorization and Notification Retiring Admission Notification Fax Numbers In this section you will find the tools and resources you need to help manage your practices prior authorization and notification requirements with program specific information available for Cardiology Oncology Radiology Clinical Pharmacy and Specialty Drugs. Once you have filled out the form you can submit it for review. Priority Health Medicare requires you or your physician to get prior authorization for certain drugs.
For prescribers only for questions regarding prior authorization or to initiate prior authorization requests call. Priority health botox prior authorization form Here are some forms you may need to help you manage your health coverage. Priority health pre authorization forms Loading 1747 downloads no ratings yet.
This means that you will need to get approval from Priority Health Medicare before you fill your prescriptions. In order to request coverage for a medication that isnt under the medical plans formulary a medical professional must fill out a prior authorization form. Easy 1-Click Apply PRIORITY HEALTH Authorization Nurse LPN job in Grand Rapids MI.
Self Referral Services Priority Partners requires notification from your provider at the beginning of your pregnancy. Chart notes are required and must be faxed with this request. Radiology advanced imaging Note.
Prior authorization information and updates Prior authorizations are expected by our members and the employers who purchase our plans to ensure the right care at the right time. Preauthorization Required The following services require pre-authorization from Priority Partners before they will be covered. Priority Health is a private company in Michigan that offers Medicare Advantage plans.
View job description responsibilities and qualifications. Priority Health Medicare requires you or your physician to get prior authorization for certain drugs. The plans provide hospitalization and medical insurance along with prescription drug coverage and other.
This form should be completed by the assessor or health care professional to provide adequate justification for the need for non-formulary to treat their patients current. Prior authorization is required for select specialty drugs through Magellan RX Management at. If you dont get approval Priority Health Medicare may not cover the drug.
Authorization Request Form FOR EHP PRIORITY PARTNERS AND USFHP USE ONLY Note. Prior authorization request and complete the spinal cord stimulator questionnaire. Prior authorization requests are defined as requests for pre-approval from an insurer for specified medications or quantities of medications before they are dispensed.
This means that you will need to get approval from Priority Health Medicare before you fill your prescriptions. Please fax to the applicable area. Priority Health reserves the right to modify these policies should circumstances warrant.
Authorization is not required for services for members who are enrolled in a Medicare-approved clinical trial. Dont worry if you. Its also a way for your health insurance company to manage costs for otherwise expensive medications.
Priority Health requires pre-authorization for certain services and procedures. On this page you can download the Priority Partners Prior Authorization Form for patients who are Priority Partners members through the John Hopkins Medicine LLC. Incomplete requests will be returned.
It is a decision by your health insurer or plan that a health care service treatment plan prescription drug or durable medical equipment is medically necessary. Easy 1-Click Apply PRIORITY HEALTH Patient Services Representative Prior Authorization 4100 Lake Drive - DME job in Grand Rapids MI. The following prior authorization provisions apply to all Individual and Group Market health plans and Medicaid and Medicare Advantage plans.
Prior authorization is a process used by some health insurance companies in the United States to determine if they will cover a prescribed procedure service or medication. Priority Partners does not require pre-authorization when you receive the services listed below or when you. Providers must submit clinical documentation in writing that explains why the proposed procedure or service is medically necessary.
Prior authorization is designed to help prevent you from being prescribed medications you may not need those that could interact dangerously with others you may be taking or those that are potentially addictive. See if you qualify. View job description responsibilities and qualifications.
Authorization is required by AIM Specialty Health for select radiology advanced. A 90-day extension based on original authorization date of open and approved prior authorizations with an end date or date of service between March 24 2020 and May 31 2020 for services at any care provider setting. All fields are mandatory.
 Priority Health Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Priority Health Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
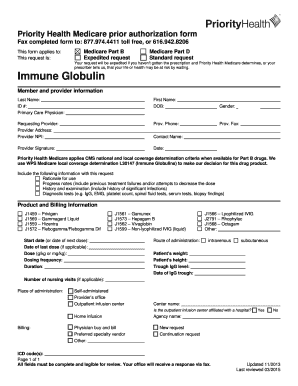 Fillable Online Ivig Prior Authorization Form Priority Health Fax Email Print Pdffiller
Fillable Online Ivig Prior Authorization Form Priority Health Fax Email Print Pdffiller
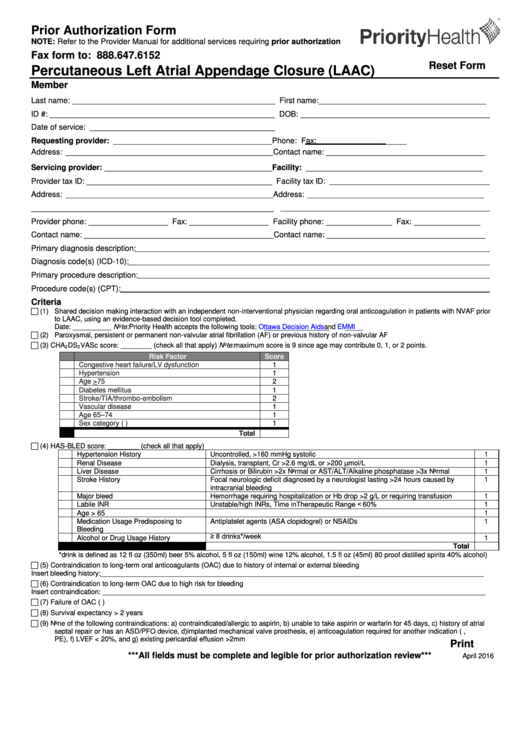
 Prior Authorization Form Priorityhealth Download Fillable Pdf Templateroller
Prior Authorization Form Priorityhealth Download Fillable Pdf Templateroller
 Top 5 Priority Health Prior Authorization Form Templates Free To Download In Pdf Format
Top 5 Priority Health Prior Authorization Form Templates Free To Download In Pdf Format
 Humira Patient Enrollment Form New Top Priority Health Prior Authorization Form Templates For Humira Models Form Ideas
Humira Patient Enrollment Form New Top Priority Health Prior Authorization Form Templates For Humira Models Form Ideas
 Priority Health Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Priority Health Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
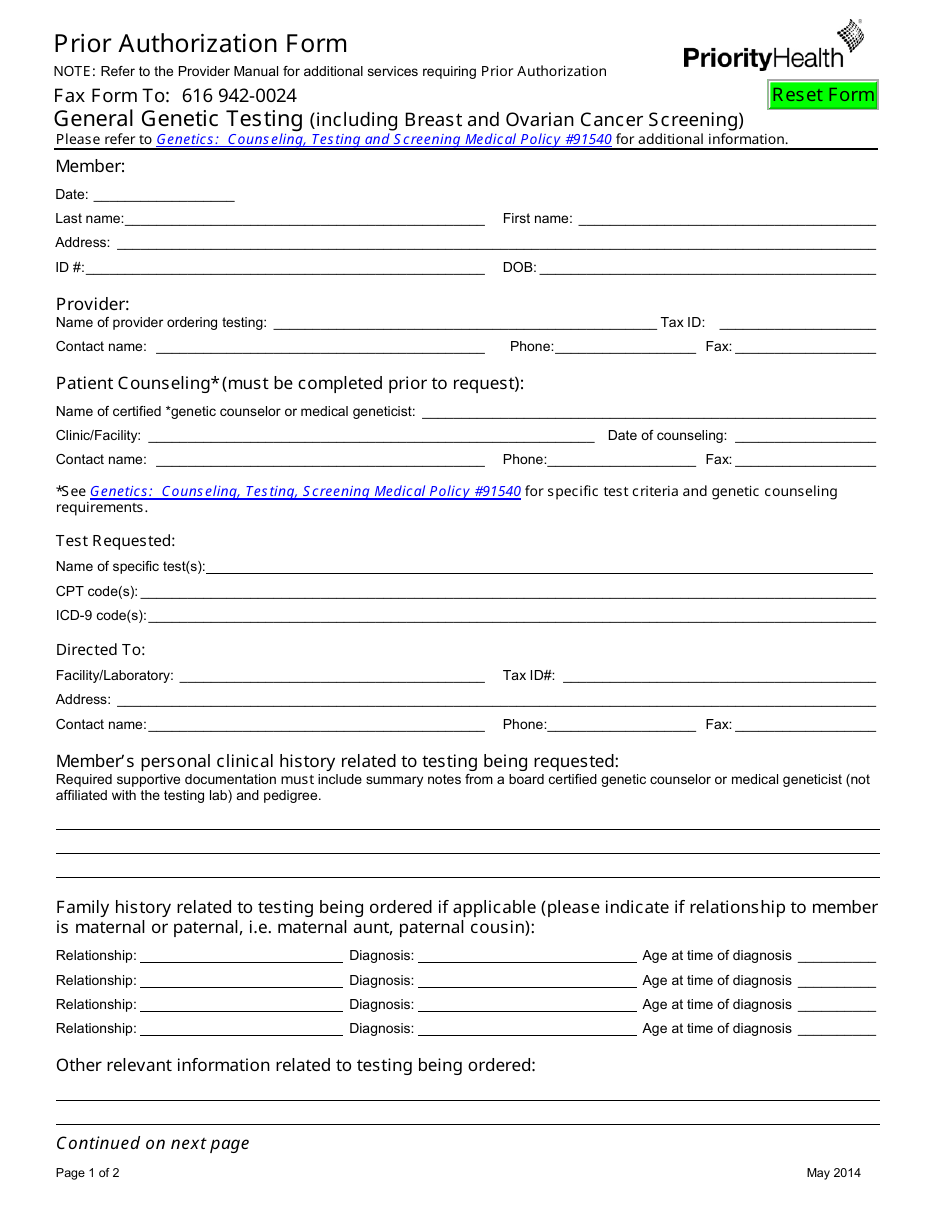
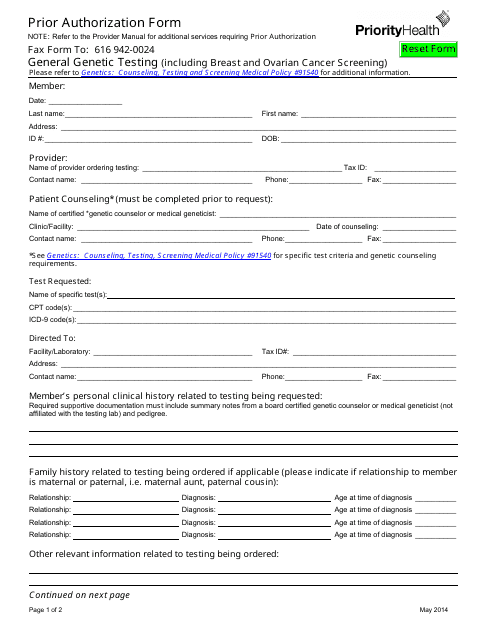
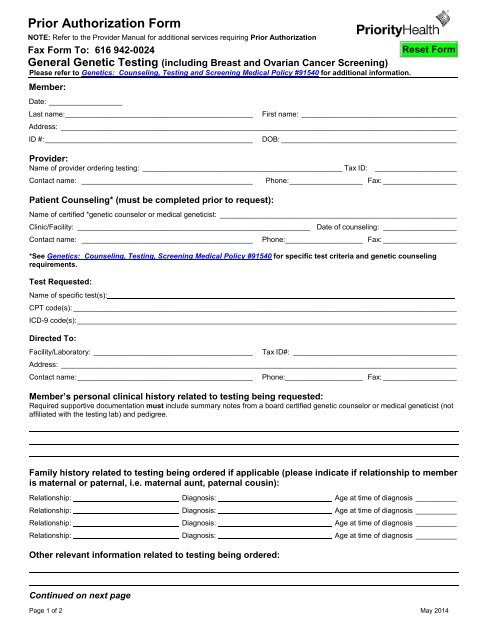 General Genetic Testing Pa Form Priority Health
General Genetic Testing Pa Form Priority Health
Https Www Evicore Com Media Files Evicore Microsites Implementation Priority Health Priority Health Lab Services Provider Orientation V6 Pdf
 Fillable Online Prior Authorization Form Priority Health Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Priority Health Fax Email Print Pdffiller
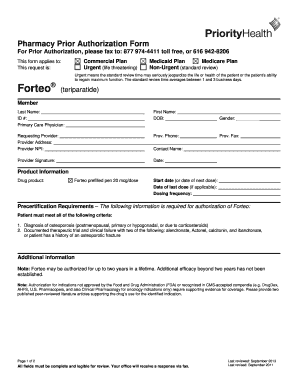
 Priorityhealth Prior Prescription Rx Authorization Form Authorization Forms
Priorityhealth Prior Prescription Rx Authorization Form Authorization Forms
 Fillable Online Prior Authorization Form Priority Health Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Priority Health Fax Email Print Pdffiller
 Prior Authorization Form Priorityhealth Download Fillable Pdf Templateroller
Prior Authorization Form Priorityhealth Download Fillable Pdf Templateroller
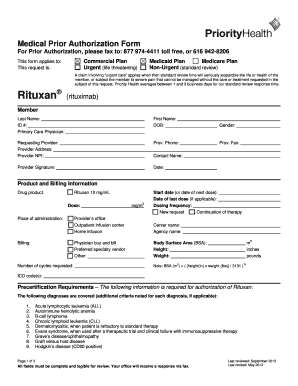
 Priority Health Medical Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Priority Health Medical Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
 Fillable Online Prior Authorization Form Priority Health Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Priority Health Fax Email Print Pdffiller
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment