Featured
- Get link
- X
- Other Apps
How Long Does Prior Authorization Take For Medication
Why does prior authorization take so long. Prior authorization is often used with expensive prescription drugs.
 Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
On an annual basis that is nearly 853 hours consumed by prior-authorization tasks.
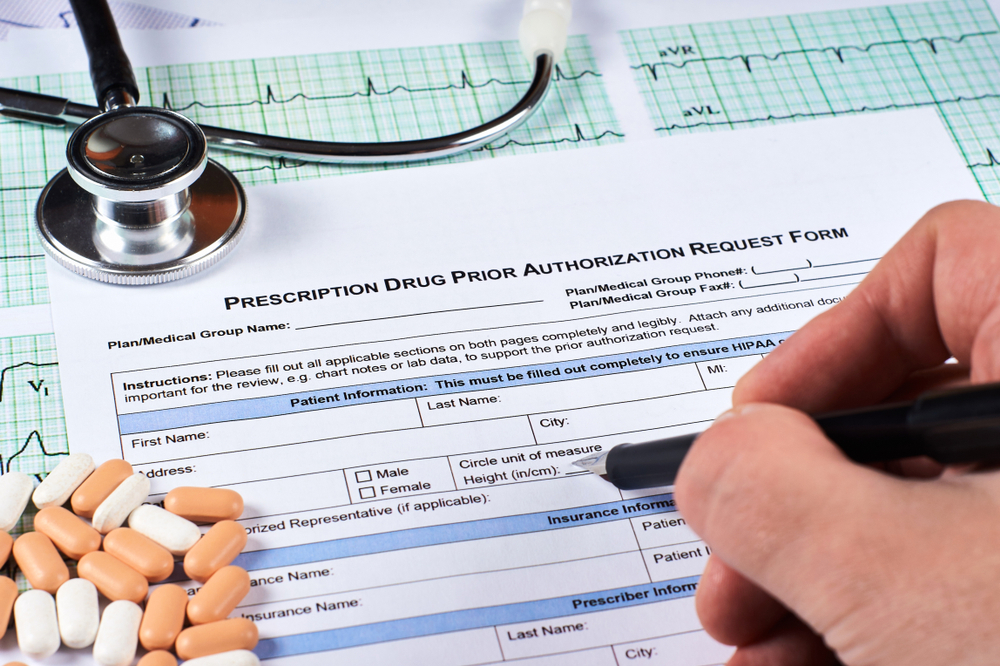
How long does prior authorization take for medication. The most worrying statistics revealed in this survey were that 24 of physicians reported that PAs have resulted in adverse events in patients due to the delay of medication receipt. Within a week you can call your pharmacy to see if the prior authorization request was approved. Prior Authorization Frequently Asked Questions Overview 1.
How Long Does Prior Authorization Take. In 2009 one study estimated that on average prior authorization requests consumed about 20 hours a week per medical practice. Remember if you are approved a prior authorization only lasts for a set period of time and you will likely have to re-apply again for future fills.
Additionally a survey by the AMA found that 69 percent of physicians wait several days just to get a response on a prior authorization request for medication. Insurance providers typically reply to a request for prior authorization within 30 business days. Depending on the complexity of the prior authorization request the level of manual work involved and the requirements stipulated by the payer a prior authorization can take anywhere from one day to a month to process.
How Long Does it Take to Get Prior Authorization for a Prescription. Prior authorization PA is a requirement that your physician obtain approval from your health insurance plan to prescribe a specific medication for you. According to the 2019 AMA prior authorization PA physician survey 91 of patients experience some delay in receiving care due to lengthy prior authorization procedures.
How long does it take to get prior authorization. Your Source for Health Insurance Information. Notice of approval or denial is.
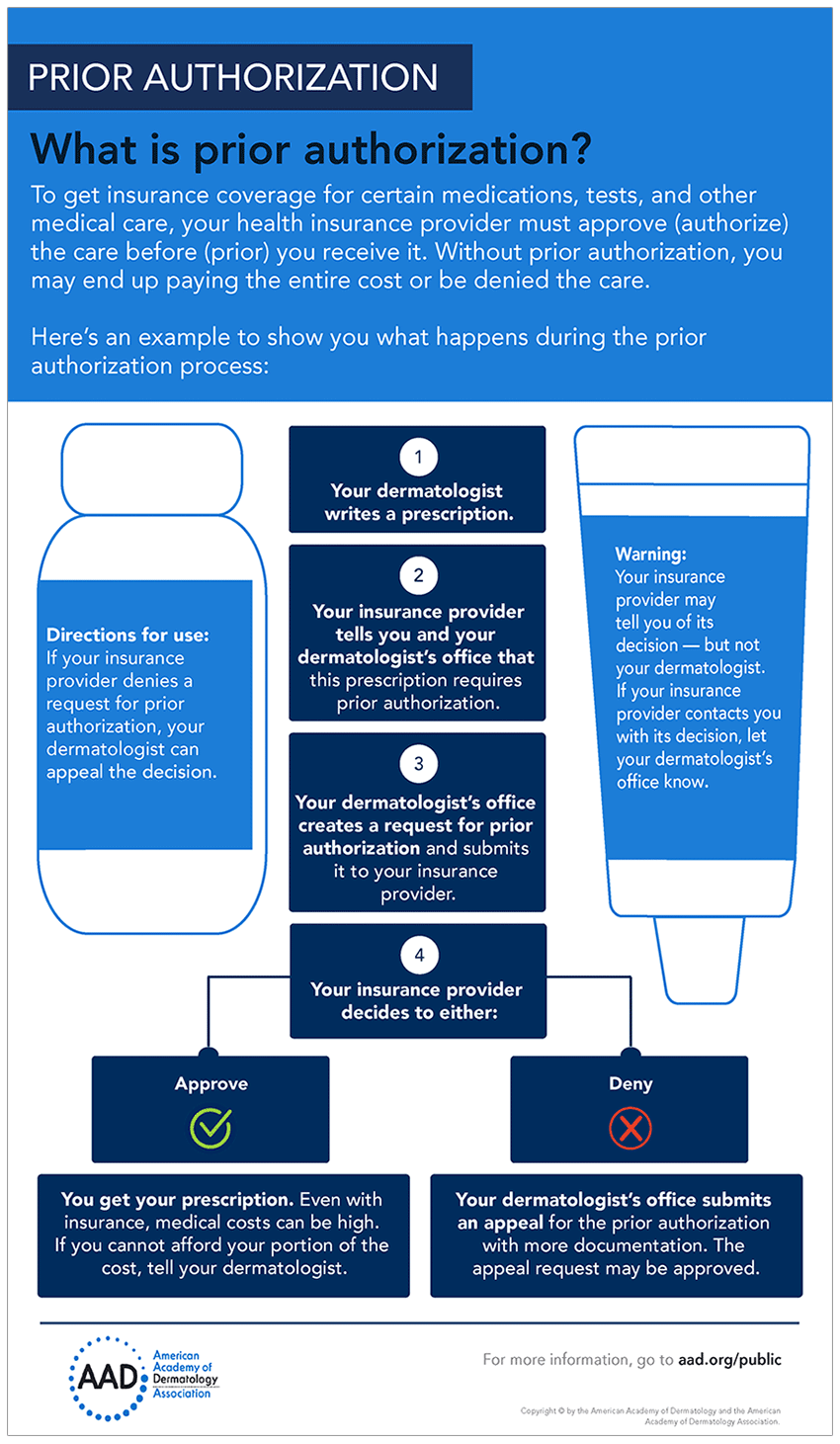
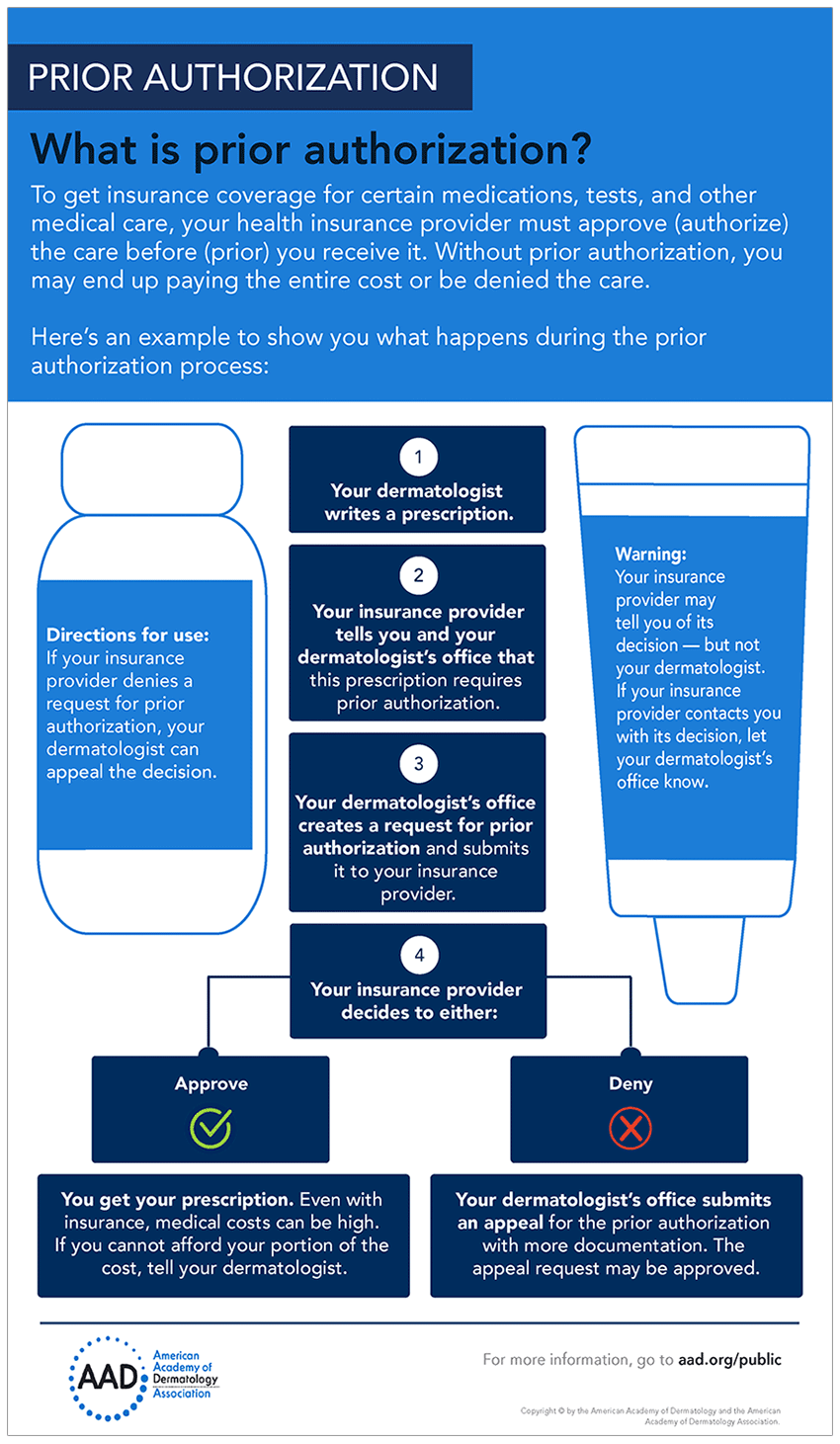
What is Prior Authorization. Prior authorization can take days to process. 24 hours to two weeks if it needs appealed.
Your insurer will then decide whether or not to cover your medicine and you should hear back from your pharmacist about their decision within two days. One hour of the doctors time nearly six hours of clerical time plus 13 hours of nurses time. Further delays occur if coverage is denied and must be appealed.
What can I do to help with the process. The company may want you to use a different medicine before they. The speed of a prior authorization can vary drastically from hours to days depending on a number of factors.
Typically we ask patients to expect 48-72 hours before approval or denial is determined by your insurance company. Although if youre waiting for a drug you should call your local pharmacy within a week. Once your provider submits the request for pre-approval to Priority Health or Cigna Payer Solutions for those living outside of Michigan it can take up to 14 days to be reviewed.
It means that your doctor must explain that the drug is medically necessary before the insurance company will cover it. Because there are few standard procedures or forms for submitting prior authorization requests confusion and frustration with the process are common among healthcare professionals. The survey found that an average of 164 hours of physician and staff time each week is spent on completing PA requirements to get patients the medicines medical services or procedures they need.
These factors include things like how it was submitted call fax etc when it was submitted the length of the review process whether additional information is needed etc. How long does a prior authorization take. -Contact you prescribers office to let them know the medication requires prior authorization.
The AMA also reported that more than 60 of physicians said they needed to wait at least one business day to complete prior authorizations while 30 said they have had to wait three business days or longer to get a response on a prior authorization request. A much faster method would be to contact your insurance company and ask what the formulary medication is. If it wasnt you can call your insurance company to see why the authorization was delayed or denied.
Sometimes its a simple as changing the prescription from capsules to pills. It can take days to get prior authorization. Ask your doctor if t.
Prior authorization is a program that monitors certain prescription drugs and their costs to get you the medication you require while monitoring your.
 Drug Channels Taking Specialty Prior Authorization From 5 Days To 5 Minutes
Drug Channels Taking Specialty Prior Authorization From 5 Days To 5 Minutes
 Charm Ehr Electronic Prior Authorization Epa
Charm Ehr Electronic Prior Authorization Epa
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
 Prior Authorizations The Pros The Cons And What To Expect In 2021 Electronic Health Record News Drchrono Blog
Prior Authorizations The Pros The Cons And What To Expect In 2021 Electronic Health Record News Drchrono Blog
 Cvs Specialty What Is A Prior Authorization
Cvs Specialty What Is A Prior Authorization
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 The Hot Potato Of Healthcare Prior Authorization Training
The Hot Potato Of Healthcare Prior Authorization Training
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
![]() Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 My Pharmacist Says He Needs Prior Authorization What S That All About
My Pharmacist Says He Needs Prior Authorization What S That All About
 How To Get Prior Authorization For Medical Care
How To Get Prior Authorization For Medical Care
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment