Featured
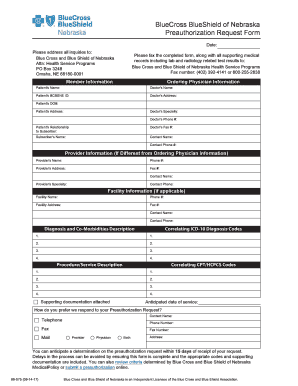
Blue Cross Blue Shield Of Nebraska Prior Authorization Form
Requests will be confidentially reviewed according to payment criteria developed by Blue Cross in consultation with independent health care consultants. Initial Request C o n tinua R ewal R ques Reason for request check all that apply.
Https Www Nebraskablue Com Media Files Nebraskabluedotcom Member Services Managing Medications Prescription Drug List Prescription Drug List 63 2296ine Ashx La En Hash 1bcf88df46fd36b28cd4be8538fa2f22e4dd21c6
Including lab and radiology related test results to.
Blue cross blue shield of nebraska prior authorization form. This form is being used for. You can submit the form by mail or fax to BCBSTX. Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity.
The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. You can find detailed instructions on how to file an appeal in the Disputed Claims Process document. Anthem Blue Cross and Blue Shield in New Hampshire.
Please send the completed form along with all supporting medical records Date. The following guidelines apply to Anthem Blue Cross and Blue Shield Anthem products issued and delivered by Anthem in New Hampshire. However out-of-network providers are not contracted with us and have not agreed to accept this responsibility.
During this time you can still find all forms and guides on our legacy site. Certain medical services and treatments need approval before you receive care. This is called prior approval precertification or preauthorization.
If you do not obtain prior approval there may be a reduction or denial of your benefit. An in-network health care provider will request a prior authorization on your behalf. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost.
Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Please use the Preauthorization Request Form or call the customer service phone number on the back of the members BCBSNE ID card. For information on precertification requirements for those members of National.
Fill out a transition of care form. Non-Formulary Exception and Quantity Limit Exception PDF 129 KB Prior AuthorizationCoverage Determination Form PDF 136 KB Prior Authorization Generic Fax Form PDF 173 KB Prior Authorization Urgent Expedited Fax Form PDF 126 KB Tier Exception PDF 109 KB. We encourage you to verify that a Prior Authorization has been approved BEFORE you receive services or supplies that require a Prior Authorization.
BlueCard appeal submission - For out-of-area BlueCard members appealing the home Blue plan. Precertificationprior authorization is required prior to being rendered. For ERS or TRS participants refer to specific form links above Form.
We are currently in the process of enhancing this forms library. 5-2016 SUBMISSION INSTRUCTIONS GENERAL PRESCRIPTION DRUG COVERAGE AUTHORIZATION REQUEST FORM This form is for authorization of prescription drug benefits only and must be COMPLETELY filled out. If you are approved for transition of care in-network benefits may be available for up to 90 days after your provider leaves the network.
Download a form from the Forms Resources section of the Evicore website and fax it to 1-888-693-3210. ABA Clinical Service Request Form. Member authorization is embedded in the form for providers submitting on a members behalf section C.
Box 3248 Omaha NE 68180-0001. Health Service Programs PO. We review them to ensure they are medically necessary.
ABA Initial Assessment Request. Supervision via Telehealth Request Attestation. Prior Authorization Step Therapy Formulary Exception.
Prior Authorization Requests Prior Authorization is a pre-approval process to determine if certain prescription drugs will be reimbursed under a members benefit plan. If you need preauthorization contact eviCore in one of three ways. Be sure to save as after you have filled out the form.
Applied Behavior Analysis ABA forms. Call 1-888-233-8158 from 800 am. To 900 pm Eastern Monday through Friday.
Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. For questions and issues regarding the new preauthorization tool please contact. Blue Cross and Blue Shield of Nebraska Preauthorization Request Form.
Find authorization and referral forms. To find out if you qualify for transition of care BCBSTX may need to request medical information from your current providers. Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review.
Precertificationprior authorization can help avoid unnecessary charges or penalties by helping to ensure that the members care is medically necessary and administered at an appropriate network facility and by a network provider. Behavioral Health for Other BCBSTX Plans. Provider Forms Guides.
Blue Cross and Blue Shield of Nebraska Attn. Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location. GENERAL INFORMATION Patient Name Request.
An Independent Licensee of the Blue Cross and Blue Shield Association MKT-148 Rev. View our individual plans page for additional appeal forms. Authorized Representative Designation Form Use this form to select an individual or entity to act on your behalf during the disputed claims process.
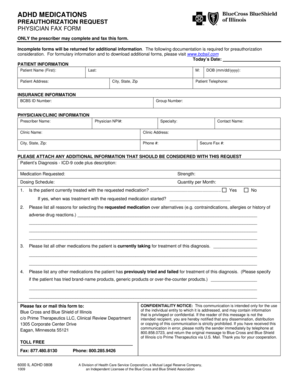
MASSACHUSETTS STANDARD FORM FOR MEDICATION PRIOR AUTHORIZATION REQUESTS Some plans might not accept this form for Medicare or Medicaid requests.
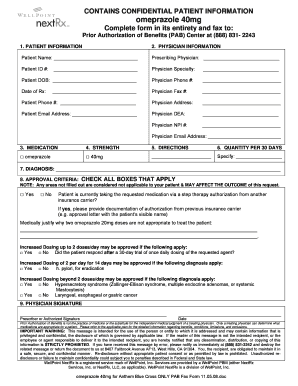 Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
 2017 2021 Form Ne Bcbsne 89 075 Fill Online Printable Fillable Blank Pdffiller
2017 2021 Form Ne Bcbsne 89 075 Fill Online Printable Fillable Blank Pdffiller
Https Www Nebraskablue Com Media Files Nebraskabluedotcom Providers Forms Preauthorization Preauthorization Request Form 89075 Ashx
 Prime Therapeutics Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Prime Therapeutics Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Https Www Nebraskablue Com Media Files Nebraskabluedotcom Providers Prior Authorization Clear Coverage Faq Ashx La En Hash D00d8accf8ee1d586c94cce150765e651da3fd68
 Blue Cross Will Soon Require Notification On Day 1 Of Admission To A Hospital Live Well Nebraska Omaha Com
Blue Cross Will Soon Require Notification On Day 1 Of Admission To A Hospital Live Well Nebraska Omaha Com
 Fillable Online Bcbsne Pre Authorization Request Form 89 075 10 15 15 Fax Email Print Pdffiller
Fillable Online Bcbsne Pre Authorization Request Form 89 075 10 15 15 Fax Email Print Pdffiller
Https Www Nebraskablue Com Media Files Nebraskabluedotcom Providers Pharmacy Management General Medication Fax Form 89074 Ashx La En Hash 64ad2e125dba671412c1928fecbcb82c2bdfc79b
 Bcbsne Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Bcbsne Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Https Www Nebraskablue Com Media Files Nebraskabluedotcom Providers Prior Authorization Clear Coverage Provider Quick Start Guide Radiology Ashx La En Hash 3ad8005a3d4cd75993f0773012ac1e50588aa21b
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Https Www Nebraskablue Com Media Files Nebraskabluedotcom Providers Forms Preauthorization Preauthorization Request Form 89075 Ashx
 2017 2021 Form Ne Bcbsne 89 075 Fill Online Printable Fillable Blank Pdffiller
2017 2021 Form Ne Bcbsne 89 075 Fill Online Printable Fillable Blank Pdffiller
 Fillable Online Prior Approval Request Authorization Form Blue Cross Blue Shield Fax Email Print Pdffiller
Fillable Online Prior Approval Request Authorization Form Blue Cross Blue Shield Fax Email Print Pdffiller
Popular Posts
Firstgroup America Benefits Enrollment
- Get link
- X
- Other Apps
Comments
Post a Comment